The testing of visual acuity in infants and children has been treated separately from the testing of adults because infants and children often can’t be tested with the same materials and techniques.
Infants vision generally improves rapidly during the first postnatal year.
Visual acuity in preverbal infants is defined as a motor or sensory response to a threshold stimulus of known size at known testing distance.
In preliterate but verbal children, visual acuity is defined as a smallest target of known size at known testing distance correctly verbally identified by a child.
Infants and children younger than 3years usually cannot identify letters or symbols verbally or by matching. So, the most successful way to assess their visual acuity is through observation of their visual systems electrophysiological responses or eye movement response to repetitive granting or checkerboard patterns . This strategy of assessing an infants resolution acuity may underestimate the depth of same visual acuity deficits but it currently provides the best method for assessing a young child’s visual capability
The visual acuity of school age children can usually be tested using standard letter acuity tests that are designed for use with adults.
Testing of preschool age children after requires modified visual acuity tests composed of a limited subset of letters or symbols that can be identified or matched to a card that is held by the child.
Visual acuity from Birth up to 3 months
At birth, visual acuity is 1/60 which improves very fast to 2/60 at 1 month and 6/60 at 4 months, with 1/60 vison the child is able to fix a face moving within 1 metre. So, visual acuity in a newborn and infant upto 3 months of age can be determined by the tests are given below :
- Blink Reflex Test : It is present since birth. When bright light is shown, a normal infant should respond by blinking.
- Pupillary Light Reflex Test : This reflex is present in premature babies over 29-31 weeks of gestational age. It is performed in a semi dark room because the infants pupil are smaller than that of normal adult and constrict in the presence of bright light in the room. In this room pupil comes to a state of semidilatation that reacts briskly. Visualization in very young children sometimes requires a magnifying glass ,as their pupils are smaller than those of the older children and the light responses are of small amplitude.
- Vestibulo Ocular Reflex Test (VOR) : It is generally tested by turning the newborns head on his/ her long axis and observing for the doll’s eye response ( deviate opposite to the direction of head rotation)
- Eye Popping Test : Eye popping reflex indicates at least the baby’s ability to detect changes in the room illumination. When the room light’s are suddenly dimmed, the baby’s upper eye lids should pop open wide for a moment. The baby will often close it’s eyes when the light’s are brought up back. This behaviour is documented as positive eye popping.
- OKN Test : It’s a method for uncooperative children as well as adults. In this test nystagmus is elicited by passing a succession of black and white stripes by means of OKN drum of the size of 10×8 inches in diameter, which is rotated at 8-10rpn through the patients field of vision. OKN is asymmetric in newborns and becomes symmetric by 4-6 months of age.
- VER : It refers to electroencephalographic (EEG) recording made from the occipital lobe in response to visual stimuli .
Visual acuity from 3-6 months
Since the fixation develops to moving objects by 3-4 months of age, the visual acuity in this age group can be assessed by the mentioned tests
- Fixation behaviour Test : Ability of the child to fix and follow the face of the examiner, toys or interesting object.
- CSM method : ‘C’ refers to the central corneal light reflex as the patient fixates eye on the examiner light and if fixation target is viewed ecentrically then it is termed as uuncentral. ‘S’ refers to the steadiness as the examiner’s light is motionless and then it is slowly moved out. ‘M’ refers to the ability of patient to maintain alignment, first with one eye then with another.
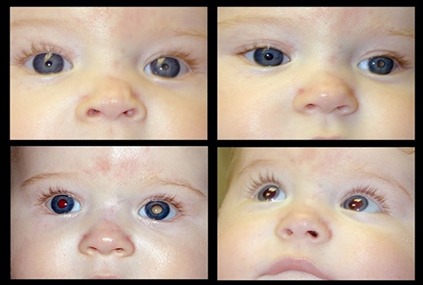
- Bruckner’s red reflex Test : In Bruckner’s red reflex test, fixa- tion and binocular comparison of the red reflex is done. The examiner should stay far enough to illuminate both pupils by the same direct ophthalmoscope beam. The examination should be carried out in dim illumination and the child’s attention to be fixed at a distance. Assess the red reflex both before and after dilatation to see how much of the pupillary space is obscured. An overall whitening of the red reflex across the entire pupil of one eye indicates strabismus or anisometropic amblyopia.
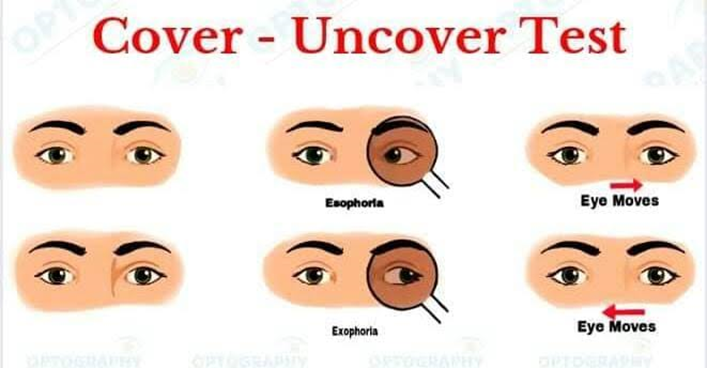
- Cover Test : This test is needed if there is a concern about strabismus. In patients with normal vision, both eyes look at an object at the same time. Therefore, if one eye is occluded, the opposite eye should not move. In patients with strabismus one eye is deviated. If the straight eye is covered, the other eye will make a movement to line up the visual target. If a patient is exo- tropic, the eye will make an inward movement. If an eye is esotropic, it will make an outward movement.
Visual acuity from 6-12 months
The tests are more useful in this age group.
A .Preferential Looking Test :
- Most Commonly used Test
- Based upon turning of the head or eyes towards the pattern rather than a uniform [homogenous] field.
- Alternating Black and White Stripes are present
- Stripe width progressively narrows which is then randomly shown next to plain test object
- Children with better vision are able to see finer grating and turn towards it.
B .Teller acuity card Test : This test is modification of PLT. This is simple to perform and very reliable and efficient test. The testing distance varies with age of the child, like the test being performed at 36 cm in infants and toddlers, at 54 cm in children up to 3 years and at 84 cm in adults. There are 17 cards, on one half of each card is a set of vertical black-and-white bars of varying size which form the pattern stimulus and on the other half, a uniform grey background which is the blank target (Fig. 2.5). In the centre of each card there is a small hole through which the examiner observes the infant’s fixation. In this by varying the spatial frequency of the bars shown, the finest bar which can no longer be resolved by the infant is used to determine the vision as the infant no longer shows the preference for patterned stimulus. This test can be used effectively on neurologically im- paired children.
Visual acuity determined with this method has been reported to range from approxi- mately 6/240 in the newborns to 6/60 at 3 months and 6/6 at 36 months of age. It must be well understood that grating acuity testing cannot automatically be equated with acuity testing based on recognition task, such as nam- ing pictures or Snellen’s letters. In normal children, grating acuity is better than recogni- tion acuity. Further, it has been suggested that different neural processing mechanisms in the brain are involved with spatial discrimination and recognition tasks. Hence, it is not advis- able to equate grating acuity with recognition acuity (Snellen’s).