- What is Heterophoria?
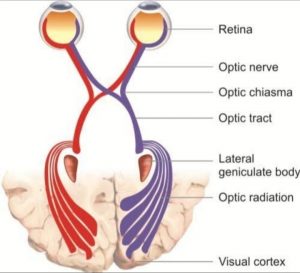
- Heterophoria is the latent muscular deviation of the eyes, which is held in position by the faculty of fusion (The 2nd grade of binocular single vision). It cannot be diagnosed until and unless the probe tests are performed to diagnose them. It is a Binocular process.
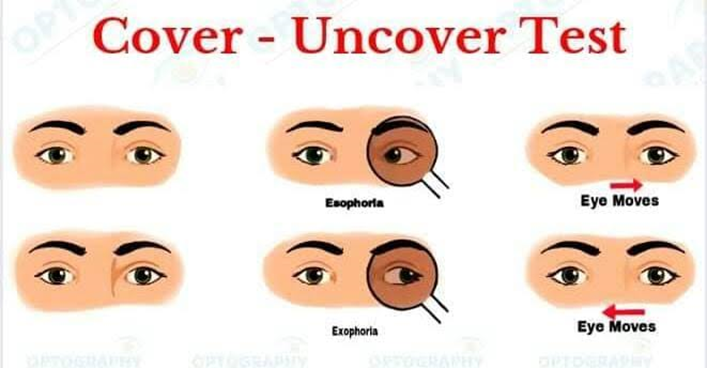
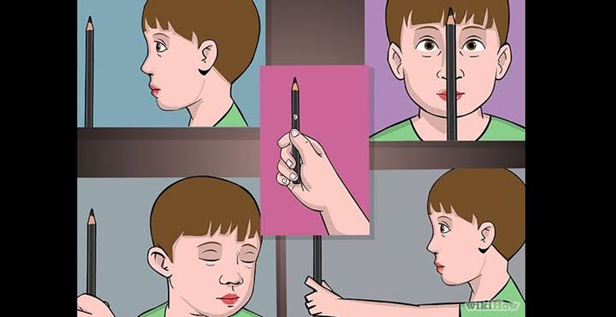
The simplest way to break fusion is by covering one eye and seeing the movement of that eye when the cover is removed (cover test).
- Two Possibilities:
- The covered eye upon uncover shows no movement –> Orthophoria.
- The covered eye upon uncover shows movement –> Heterophoria.
- Covered eye upon uncover moves from the temporal side to the nasal side –> Exophoria.
- Covered eye upon uncover moves from the nasal to the temporal side –> Esophoria.
- Classifications or Types of Heterophoria
- Horizontal Heterophoria
- Exophoria: Exophoria is a condition in which your eyes drift outward when fusion cannot overcome the deviation. It usually appears for a short time while you are doing certain types of tasks and only visible when testing eye position and breaking fusion. It’s a latent type deviation.
- Esophoria: Esophoria is an inward turn or deviation of the eye that eye that only occurs some of the time. Eyes appear to work together normally in patients with esophoria, but if the fusion, or binocular interaction between the eyes is broken, an inward deviation then can appear.
- Vertical Heterophoria
- Hyperphoria: Hyperphoria is an upward turn or deviation of the eye that only occurs some time. It’s a latent strabismus in which the visual axis of one eye deviates upward in relation to the other.
- Hypophoria: Hypophoria is downward turn or deviation of the eye that only occurs some time. It’s a latent strabismus in which the visual axis of one eye deviates downward in relation to the other.
- Torsional Heterophoria (Cyclo phoria)
- Incyclophoria: The tendency of the eyes to rotate inward. Prevented by the impulse of the eyes to act in coordination is called Incyclophoria. Also called as minus-cyclo phoria.
- Excyclophoria: The tendency of the eyes to rotate outward. Prevented by the impulse of the eyes to act in coordination is called Excyclophoria. Also called as plus-cyclophoria.
- Investigations of Heterophoria
Cover / uncover and alternative cover test (Qualitative Analysis)
- Done both at 6 mts and 40 cms (at distance & near)
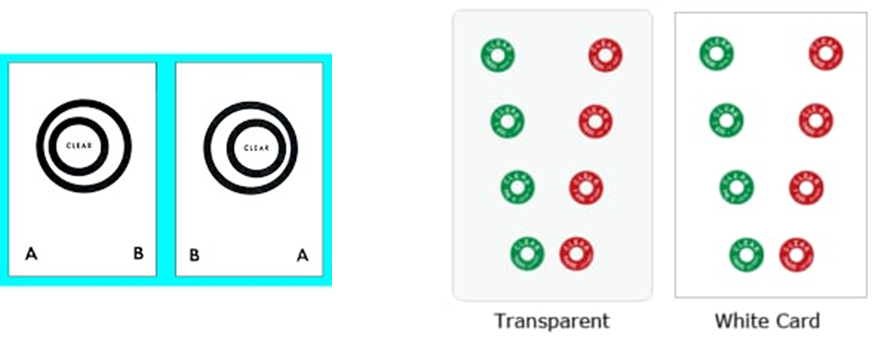
Maddox Rod test and Maddox Wing test (Quantitative Analysis)
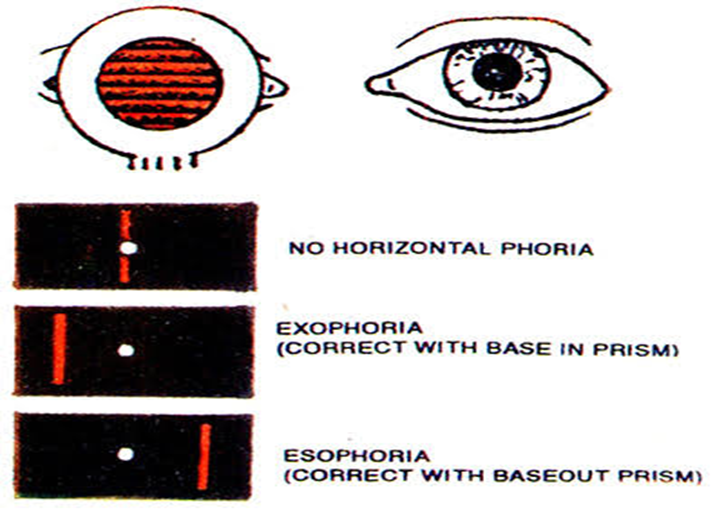
- Maddox Rod is done at 6mts (distance test)
- Maddox wing / Howell phoria Card test is done at 40 cms (Near test)

- The amount of Heterophoria can remain same or vary at distance and near. If the amount remains same at distance and near, it is called basic Exophoria or basic Esophoria.
- Relationship with Ametropia
- Horizontal phoria responsible for all vergence dysfunctions and these two phorias (Exophoria and Esophoria) are associated with all refractive errors. Vertical or torsional phoria have no particular affinity for any refractive error. Some textbooks relate torsional phorias to be associated with oblique Astigmatisms.
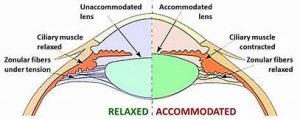
- Uncorrected Hyperope: over-accommodation at both distance and near in order to achieve normal visual acuity. This will lead to simultaneous over-convergence, which can lead to latent inward deviation of the eye, which is called Esophoria.
- Uncorrected Myope: Distance acuity is subnormal. There is no accommodative-convergence demand either for distance or for near, which can lead to latent outward deviation of the eyes, which is called Exophoria.
- Horizontal Heterophoria and The Vergence Dysfunctions
- Vergence dysfunctions are always related to Convergence and Divergence anomalies in NSBD analysis and the primary clinical information is derived from the amount of Horizontal Heterophoria at distance and near.
- Exophoria relates to stimulation of Divergence controlled by fusional faculty.
- Esophoria relates to stimulation of convergence controlled by fusional faculty.
- Heterophoria with good fusional control is termed as compensated Heterophoria and where the fusional control is partial or lost, then the term Decompensated Heterophoria is applied. Decompensated Heterophoria can lead to NSBD and in extreme cases, Heterophorias (Manifest Squint).
- Vergence Dysfunctions:
- Basic Exophoria (Distance Exo = Near Exo)
- Basic Esophoria (Distance Eso = Near Eso)
- Convergence Insufficiency (C.I) –> (Near Exo > Distance Exo)
- Convergence Excess (C.E) –> (Near Eso > Distance Eso)
- Divergence Insufficiency (D.I) –> (Distance Eso > Near Eso)
- Divergence Excess (D.E) –> (Distance Exo > Near Exo)
- Vertical Heterophoria (Less Common)
- Accommodative Disorders:
- Accommodative Insufficiency (A.I)
- Accommodative Excess (A.E)
- Accommodative Infacility (A.Inf).
- Possible Examination for Heterophoria
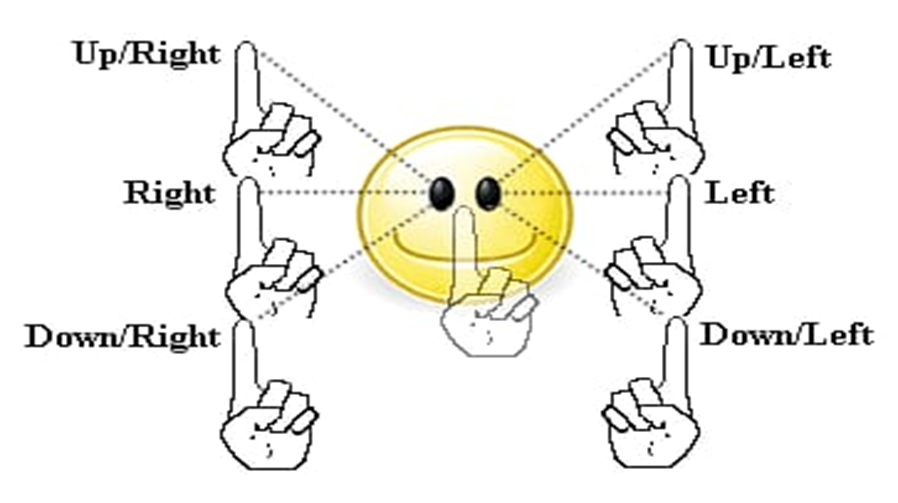
- EOM (Extra Ocular Movement): The primary aim of EOM is to focus an image of an object of interest on the fovea, the region responsible for sharp central vision, and keep it steady. This is accomplished through two distinct types of eye movements namely gaze holding (Involuntary) and gaze shifting (voluntary) eye movement. The former system includes five types of eye movements (smooth pursuit, vestibular, optokinetic, fixation and vergence), all of which need some kind of stimulus and are involuntary. The letter includes only one type of eye movements, which is called saccadic eye movements, which are voluntary. Saccades and smooth pursuit eye movements are two different modes of oculomotor control. Saccades are primarily directed toward stationary targets whereas smooth pursuit is elicited to track moving targets.
Near point of Convergence (NPC): The point is of intersection of the lines of sight of the eyes when maximum convergence is utilized. This point is called Near Point of Convergence(NPC)
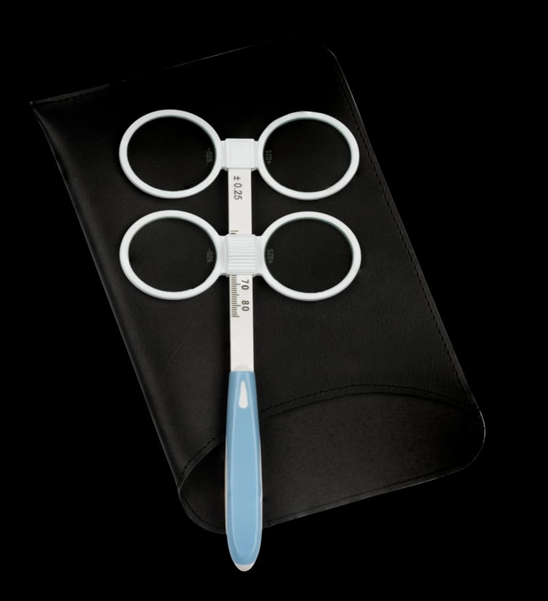
RAF Near Point Rule (RNPR) is a routinely used instrument in optometry practice to measure the Near Point of Convergence (NPC). The measurement of NPC is an important criterion for diagnosis and management of Convergence insufficiency. The RNPR forms an important tool for Opthalmic clinicians however, only a very little is understood about it.
- Gradient AC/A Ratio: It is a simple and effective clinical method.Accommodation is either stimulated or relaxed by 1.00 diopter by using a ‘-1.00 D’ or ‘+1.00D’ binocularly and the change in near phoria is noted.Morgan classified AC/A ratio into Normal/Low/High AC/A
Normal AC/A: 4/1
High AC/A: >6/1
Low AC/A: >= 2/1
- The test for measuring the fusional vergence are by:NFV/NRC –> Negative Fusional Vergence / Negative Relative Convergence.
This is the ability of a person to relax Fusional Convergence or the ability to induce Fusional Divergence. It is measured by Base in Prism (∆BI).

- PFV/PRC –> Positive Fusional Vergence / Positive Relative Convergence.
This is the ability of a person to excite Fusional Convergence. It is measured by Base Out Prism (∆ BO).
- Both the NFV and PFV tests are carried out at 6mts and 40 cms (Distance and Near). Then the values are compared with the expected to arrive to a proper diagnosis.
- Test for probing accommodative relaxation and stimulation:
- NRA: Negative Relative Accommodation (NRA) test helps to relax accommodation. NRA test is done by using plus spherical lens (We have to decrease stepwise accommodation demand binocularly without suppression).
- Test for probing accommodative relaxation and stimulation:
It decreases accommodative convergence and also increases fusional convergence to maintain fusion of the stationary target.
- PRA: Positive Relative Accommodation (PRA) test helps to stimulate accommodation. PRA test is done by using minus spherical lens (We have to increase stepwise accommodation demand binocularly without suppression).
It increases accommodative convergence and also increases fusional divergence to maintain fusion of the stationary target.
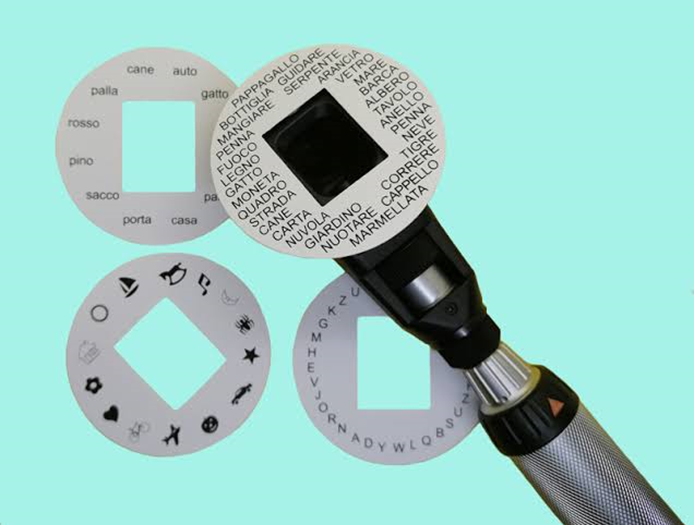
- Test for probing accommodative flexibility:Accommodative Facility: This is the ability to repeatedly shift accommodative response rapidly and in a jump step. This test is performed to testing both the accommodation and vergence mechanism are at play.
- This test is done by +- 2.00D Accommodative Flipper.This test is performed at a distance of 40 cms.
- Plus lenses: Decrease accommodation in a jump step.
- Minus lenses: Increase accommodation in a jump step.
- MEM: The technique is performed monocularly. The aim is to determine the accommodative lag and lead by estimating the reflex motion without disturbing the accommodative state. The technique is particularly useful for observing a patient’s spontaneous accommodative response to a detailed target at their normal working distance.
Worth 4 dot: This is a dissociation test which can be used with both distance and near fixation and differentiates between BSV, ARC and suppression. For this patient wears goggles with red lens in front of the left eye and green lens in front of the right eye and views a box with four lights – one red, two green and one white.

- Possibilities: If BSV is present all four lights are seen.If all four lights are seen in the presence of a manifest deviation, harmonious ARC is present.If two red lights are seen, left suppression is present.If three green lights are seen, right suppression is present.If two red and three green lights are seen, diplopia is present.If the green and red lights alternate, alternating suppression is present.
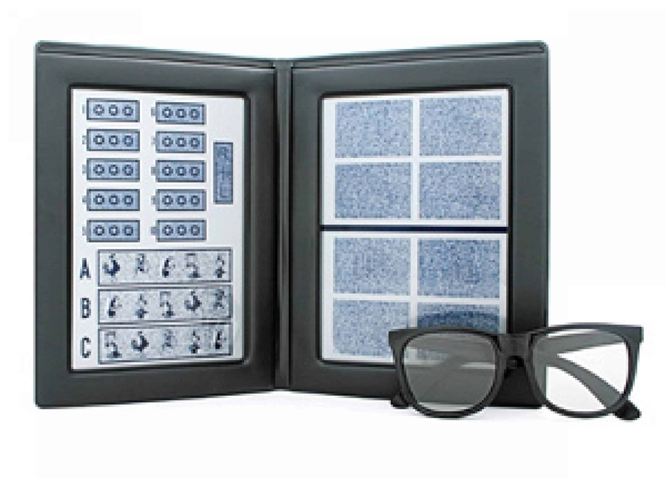
- Stereo test:
- Titmus stereo test: Recognized as the standard for stereo depth perception testing. It allows evaluation of both gross and fine stereo vision. Easy to perform polarized glasses are used to perform test.
- Stereo test:
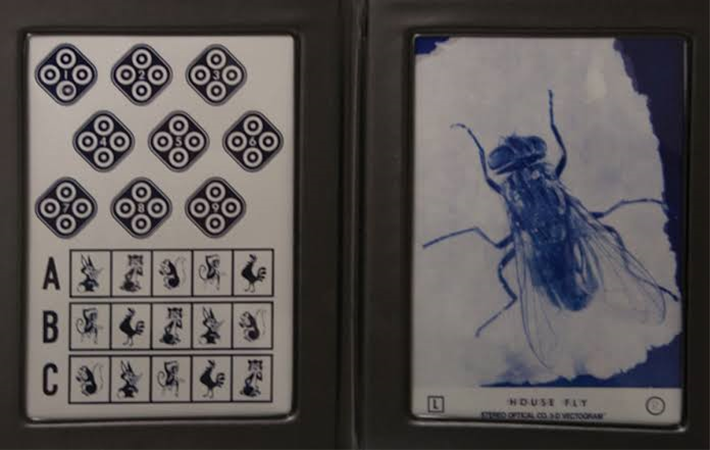
The test includes:
A fly for gross stereopsis (3000 seconds of arc)
Graded circle test (800 to 40 seconds of arc)
Animal test (400 to 100 seconds of arc)
- Randot Stereo test: The Randot Stereo test is aimed for adult stereo testing, but also includes an animal portion for pediatric testing. Adult patients are asked to identify six geometric shapes during testing. This test helps to test the patient’s depth perception along with normal stereo vision. Adult testing involves 400 to 20 seconds arc, and pediatric testing involves 400 to 100 seconds of arc.
- Clinical Expecteds in Optometry (Basic Binocular Function Assessments)
[Based on Optometric Extension Program Foundation USA and Binocular Vision Textbook of Scheiman and Wick]
- Normal NPC is 6 cms of the Nose.
- Distance Phoria 1 Exo
- Near Phoria 4-6 Exo
- Gradient AC/A: 4:1
- NFV (∆BI Range) @ 40 cms : Break 12 recovery7(Children)
- PFV (∆BO Range) @40 cms : Break 23 recovery 16 (Children)
- NFV (∆BI Range) @40 cms : Break 13 recovery 10 (Adults)
- PFV (∆BO Range) @40 cms : Break 19 recovery14 (adults)
- NFV (∆BI Range) @6 mts: Break 7 recovery 4
- PFV (∆BO Range) @6 mts: Break 20 recovery 10
- NRA (Plus Sphere) @40 cms : +1.75D
- PRA (Minus sphere) @40 cms : -2.25D
- MAF (+- 2.00 Flipper) @40 cms :
6 years -> 5 cpm
7 years -> 6 cpm
(8-12years) -> 7 cpm
(13-30 years) -> 11 cpm
- BAF (+- 2.00 Flipper) @40 cms:
6 years -> 3 cpm
7 years -> 4cpm
(8-12 years) -> 5cpm
(12-30 years) -> (8-10) cpm
- MEM Retinoscopy @40 cms: (+0.50D to +0.75D)
High MEM (Accommodative Lag) -> With or Normal Movement.
Low MEM (Accommodative Lead) -> Against or no motion
- For discerning the clinical significance the stereo acuity levels where categorized into normal (20 arc seconds or better), Borderline (25 arc seconds to 40 arc seconds) and reduced stereopsis (50 arc seconds to 400 arc seconds).
- Anomalies of Convergence and Accommodation:
- Convergence Insufficiency and Convergence Excess (C.I & C.E):
- Symptoms of C.I & C.E:
- Headache and Asthenopia
- Blurring of VA
- Occasional Diplopia
- Burning / Lacrimation / Frequent stye
- Feeling sleepy during sustained near vision activity
- Decrease Comprehension
- Words appear to move on the page
- Task Avoidance
- Basic Exo and Eso are relatively asymptomatic.
- Clinical signs of C.I (Most Common Group of NSBD):
- High near point Exophoria (Near > Distance)
- Decrease positive Fusional Vergence (∆BO Range)
- Increase Positive Relative Accommodation
- Receding Near Point of Convergence.
- Low AC/A Ratio.
- Fails Binocular Flippers (specially the Plus Side)
- Low MEM (Accommodative Lead)
- Low Hyperopic or Low myopic in nature: can lead to pseudomyopia.
- Clinical signs of C.E:
- High Near Point Esophoria (Near > Distance)
- Decrease Negative Fusional Vergence (∆BI Range)
- Decrease Positive Relative Accommodation.
- Near Point of Convergence: up to nose tip.
- Fails Binocular Flipper (Specially the Minus Side)
- High MEM (Accommodative Lag)
- Usually Hyperopic in nature.
- Treatment strategies of C.I:
- Rx for distance and near
- Added plus for C.I secondary to primary A.I
- Vision Therapy (The best choice in this case).
- Prisms in Rx:
- Vertical prisms if required for vertical deviations.
- Horizontal prisms –> not the first choice.
- Divergence Excess (D.E) and Divergence Insufficiency (D.I) are less common in clinical practice, though they are encountered.
- Accommodative Insufficiency (A.I):
- Symptoms of A.I:
- Blurred vision
- Headache
- Eyestrain
- Reading Difficulties
- Visual & General fatige
- Comprehension Decreases over time
- Avoidance of near work
- Clinical signs of A.I:
- Unable to produce sufficient accommodation for the demand
- Amplitude (For age) reduced by at least 2 Diopter
- Unable to clear ‘-2.00D’ lens in the Accommodative Flipper.
- High MEM (Accommodative lag)
- Reduced PRA (less than ‘-2.50D’)
- Low PFV (∆BO Range) at near (less than 12∆BO)
- Treatment strategies of A.I:
- Appropriate refractive correction
- Added plus at near
- Vision Therapy
- Symptoms of A.I:
- Accommodative Excess (A.E)
- Symptoms of A.E:
- Blurred vision–>worse after prolong near work
- Headache after near work
- Asthenopia
- Difficulty in changing focus: Near to far.
- Photosensitivity
- Precursor of Environmentally Induced Myopia/ Late onset myopia which is preventable.
- Clinical signs of A.E:
- Inability to relax Accommodation
- Difficulty clearing ‘+2.00D’ lenses: Monocular & Binocular.
- Low MEM (Accommodation Lead)
- Reduced NRA
- Reduced NFV (∆BI) at near (Less than 6∆BI)
- Treatment strategies of A.E:
- Refractive correction –> Consider added plus at near.
- Vision Therapy
- Symptoms of A.E:
- Accommodation Infacility (A.Inf):
- Symptoms of A.Inf:
- Blurring of vision while shifting gaze from far to near.
- Reading Difficulties
- Headache and Asthenopia
- Avoidance of near work
- Comprehension decreases over time.
- Learning problems/ Attention Deficit Hyper Activity Disorder (ADHD)
- Clinical signs of A.Inf:
- Difficulty in changing focus from near to far or vice versa.
- Decrease Monocular & Binocular facility
- Reduced PRA & NRA
- Low PFV & NFV at near
- Treatment strategies of A.Inf:
- Refractive correction with added plus
- Vision Therapy
- Symptoms of A.Inf:
- Symptoms of C.I & C.E:
- Convergence Insufficiency and Convergence Excess (C.I & C.E):
***Key point For NSBD Case***
- Common possible findings:A.I with C.E:C.E –> Near Eso > Distance EsoNPC –> up to nose tipGradient AC/A –> HighNFV –> Low, PFV–> HighNRA –> High, PRA –> LowBAF –> Low (minus side fail), MAF –> LowMEM –> Lag –> (with or normal movement)
[ Usually Hyperopic in Nature]
- A.E with C.I: C.I –> Near Exo > Distance ExoNPC –> RecedingGradient AC/A –> LowNFV –> High, PFV –> LowNRA –> Low, PRA –> HighBAF –> Low (plus side fail or difficulty), MAF –> LowMEM –> Lead –> (Against or no motion)
[Low Hyperopic or Low myopic in Nature can lead to pseudomyopia]
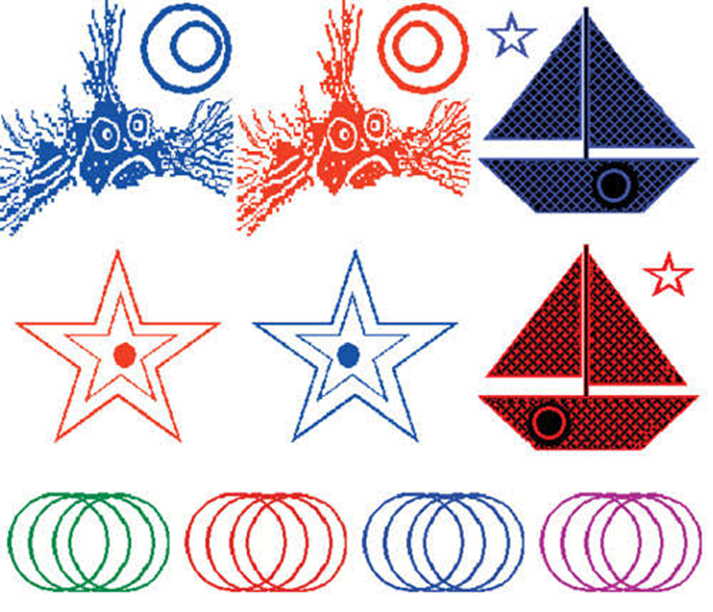
- Vision Therapy Guidelines for Vergence Dysfunction (Basic):
Pencil push-up test
Brock strings

Marsden Ball

Eccentric Circles / Life savers Cards
Balance boards / Walking Rails

Aperture Rules

Vectograms

Mirror Stereoscopes

Various Computer Based Vision Therapy Programs.
- Goals of Vision Therapy in Vergence Dysfunctions:
- Start with monocular Accommodative and Oculomotor Therapies –> then proceed to Binocular Therapies.
- Proceed to gross vergence therapies
- There after smooth and Jump vergence therapies
- Integrate Accommodation –> Vergence Relationships.
- Integrate Versions, Vergence & Accommoodation
- Anti-suppression Therapies
- Expected Goals:
- Amplitude for smooth vergence: 35∆BO & 15∆BI.
- Amplitude for jump vergence: 24∆BO & 12∆BI.
- Speed for jump vergence: Fusion within 2 seconds.
- Stamina Goal: Holding Fusion for 10 seconds repeatedly.
Summary of Treatment options in NSBD
| Types of NSBD | Primary Rx Options |
| Convergence Insufficiency | Low plus at near, BI prisms, VT. |
| Convergence Excess | Added plus near, VT |
| Divergence Insufficiency | Relieving prisms with refractive Rx, VT |
| Divergence Excess | Refractive Rx, VT |
| Basic Exophoria | Relieving prisms, Refractive modification, VT |
| Basic Esophoria | Added plus, VT |
| Accommodative Insufficiency | Added plus on refractive Rx, VT |
| Accommodative Excess | Added plus refractive Rx, VT |
| Accommodative Infacility | Refractive Rx, added plus, VT |
| Oculomotor dysfunctions | VT |
| Fusional Vergence Dysfunctions | Refractive modifications, VT |
- Required modification of Rx (Horizontal Heterophoria with Ametropia):
- Thumb Rule:
- Hyperopia + Exophoria –> Cutdown Plus Rx
- Hyperopia + Esophoria –> Full plus / consider added plus
- Myopia + Exophoria –> Optimum minus / minimum minus (MM)
- Myopia + Esophoria –> Under Correct minus / consider PAL / Bifocals / Contact lens with spectacle Combination.
- Thumb Rule:
- Example of Clinical Case Analysis (NSBD):
A 22-year-old adult comes to your clinic with the complaint of eye strain and watering with redness and itching at the day’s end. The patient is an IT professional and works on Laptop for more than 12 hours a day with minimum break. The general health is good and the medical history is unremarkable.
O/E
UV OD 6/9 OS 6/9P OU 6/9 – N6
Anterior Segment: Chronic Simple Conjunctival Congestion OU/Corneas Clear/ RRE pupils/ ROPLAS –ve/AC Depth: WNL
Posterior Segment: Discs + Maculae – WNL; HNRR (healthy neuro-retinal rim); CDR 0.4:1; A: V 2:3; FR+
Dry Retinoscopy: OU -1.00DS/-0.75DC X 90 = (-2.00DS/-0.75DC x 90)
Subjective Acceptance Dry: OU -0.50DS/-0.25DC X 90 6/6 EE
Autorefractometry: OU -3.00DS/-1.00DC X 90
- What you are going to do?
- Refractive Findings is not proportional to the degree of Subnormal VA
SO, THIS IS PSEUDOMYOPIA
- Why this patient became a patient of Pseudomyopia?
- There must be a MISMATCH between Accommodation + Convergence.
Therefore, the primary reason may be CI & AE or AE alone
- Your Examination Pattern should be:
- Ocular Motility – FFP
- Cover Test D/N – N EXO > D EXO
- Near point of Convergence (NPC) – Receding NPC – Deviation of one eye outwards
- Maddox Rod @ 6mts = 4 Exo
- Maddox Wing @ 40cms = 8 Exo
- AC/A (Gradient) = Low 2/1 (-1.00 = 6Exo)
- NFV (BI Range) = D & N NFV > PFV
- PFV (BO Range) = D & N
- NRA (+ to Blur)
- PRA (- to Blur) PRA >NRA
- MAF – minus side easy
- BAF – minus side easy / Plus side fail or difficulty
- MEM – LEAD
- W4DT TEST – NO SUPPRESSION
- STEREOACUITY –> 60 – 70 SECS OF ARC
- REFRACTION:
- Borish Delayed Refraction = +0.50DS 6/6
- Refraction with Cyclopentolate = +3.00DS/-0.25DC x 90
- PMT = -0.50DS/-0.25DC x 90 OU
- Rx:
- Accommodative Flipper VT
- NPC VT (Pencil Push Up / Cat Card)
- Brock String VT
- Rx OU +0.75DS for Near Vision Use only.
- Eye Health:
Whether the Redness is due to Chronic Conjunctivitis/Low Grade Allergic Conjunctivitis/ Tear Film Instability (Treatment according to the differential diagnosis).
- Conclusion
Heterophoria and other Non-Strabismic Binocular Dysfunctions coexist with all Ametropia as well as Emmetropia (Normal or Artificial Emmetropia) and are more prevalent that ocular pathology in routine Optometry practices. Most of these patients are examined on the basis of “Refractive Error” only and the Binocular Vision aspect is often ignored. This often leads to subtle imperfection in the total Visual Rehabilitation of a patient – particularly the Pediatric patients. Optometry has the answers to many unresolved visual problems which are symptomatic yet have negligible refractive deviation. These lead to a poor Quality of Life. In these patients, precise refractive compensation may not bring the desired relief – leading to low productivity in their lives. Learning Disability, Cerebral Palsy, Autism Spectrum Disorder and even some psychiatric problems like anxiety disorders have been associated with poor Binocular Functions – that can be assessed and remedied. Even the common Computer Vision Syndrome has all sorts of NSBD problems – where just prescribing a refractive correction and ocular lubricant might not be solving the patient’s problems.
Hence, it should be mandatory for every Optometrist to analyze Basic Binocular Functions and relate them to the Ametropia and modify the refractive compensation for better visual prognosis. These tests do not involve expensive equipment and they are easy to master with a little effort from the practitioner. If we can embrace this pattern of visual analysis, we will surely make a difference in our practices as well as establish our professional status.