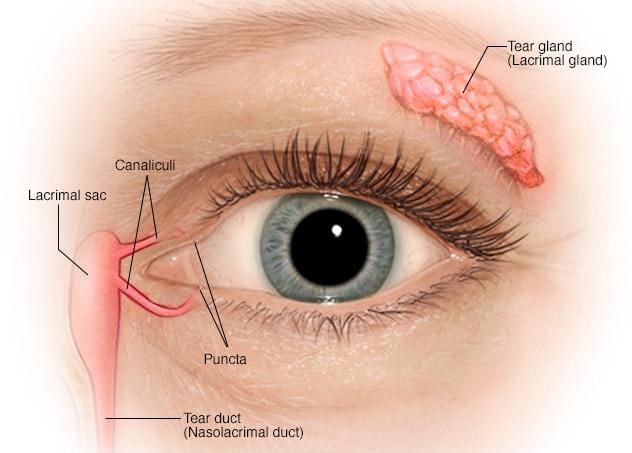
THE LACRIMAL APPARATUS:
The lacrimal apparatus comprises the structures concerned with the formation of tears (the main lacrimal gland and accessory lacrimal glands) and its transport .
The lacrimal passage includes : puncta, canaliculi, lacrimal sac and nasolacrimal duct.
LACRIMAL GLANDS
Main lacrimal glands:
The main lacrimal glands is situated in the fossa for lacrimal gland, formed by the orbital plate of frontal bone, in the anterolateral part of the root of orbit .The gland is divided in its anterior aspect by the lateral horn of aponeurosis of the levator muscles into two parts-the superior orbital and the inferior palpebral , which are continuous with each other posteriorly .
The orbital part of lacrimal gland:
- It lies in contact with the septum orbital.
- Posterior border is round and it is large, about the size and shape of a small almond. It has two surfaces (superior and inferior), two borders(anterior and posterior) and two extremities (medial and lateral).
- The superior surface of the orbital part is
convex and lies in contact with the lining the part of the frontal bone forming the fossa for the lacrimal gland. it is attached to the periorbita by fine trabeculae.
- The inferior surface of the orbital part is concave and lies the levator palpebrae superioris muscle and the lateral horn of the levator aponeurosis.
- The anterior border is sharp and seems within and parallel to the orbital margin, upto the zygomatico frontal suture. It becomes continuous with the palpebral part of the gland. It lies in the contact with the orbital pad of fat.
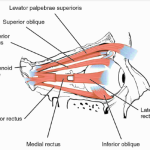
- Lateral extremity rests on the lateral rectus muscle.
- Medial extremity is related to the levator palpebrae superioris muscle.
The palpebral part of lacrimal gland
- It is small (about one -third the size of orbital part) and consist only of only two or more lobules.
- It is situated upon the course of the ducts of the orbital part from which it is separated by the levator palpebrae superioris muscle, which is related to it superiorly.
- Inferiorly the gland lies in relation to the superior fornix.
The gland is compressed from above downwards and can be seen through the conjunctiva when the upper li is everted. Posteriorly it is continuous with the orbital part.
Ducts of lacrimal glands
About 10-12 ducts pass downwards from the main lacrimal gland to open in the lateral part of the superior fornix. Since all the ducts pass through the palpebral part of the gland, therefore excision of the palpebral part alone amounts to excision of the entire gland as far as the secretory function of the gland is concerned.
Structure of the lacrimal gland
- Lacrimal gland is a branched tubulo-alveolar (serous acinous) gland, similar in structure to the salivary glands. Microscopically, it consists of glandular tissue, stroma and septa. It is lined by a capsule as the outermost limit.
- The glandular tissue consists of acini and ducts arranged in lobes and lobules separated from each other by the fibrovascular septa. The acini are lined by a single layer of pyramidal cells mounted on a basement membrane.
- These cells are surrounded by a layer of flattened myoepithelial cells. The pyramidal cells are of the serous type with eosinophilic secretory granules and a round nucleus situated towards the base.
- These cells secrete the tears, expelled by the contraction of myofibrils .The secretion of the acinar units is drained by connecting channels which to begin which are intralobular, then these become extralobular and lastly open in the ducts. The ducts are lined by the two layers of the epithelial cells , the inner lining is formed by thick cylindrical cells and the outer layer is of flattened cells.
- The stroma of the lacrimal gland is formed by the mesodermal tissue which contain connective tissue, elastic tissue , lymphoid tissue ,plasma cells , rich nerve teminals and blood cells.
BLOOD SUPPLY:
Main lacrimal gland is supplied by lacrimal artery, a branch of ophthalmic artery. Sometimes a branch of transverse facial artery may also supply the gland.
The lacrimal veins draining the gland join the ophthalmic vein.
LYMPHATIC DRAINAGE:
The lymphatic drainage is along the conjunctival drainage into the pre- auricular lymph nodes.
NERVE SUPPLY:
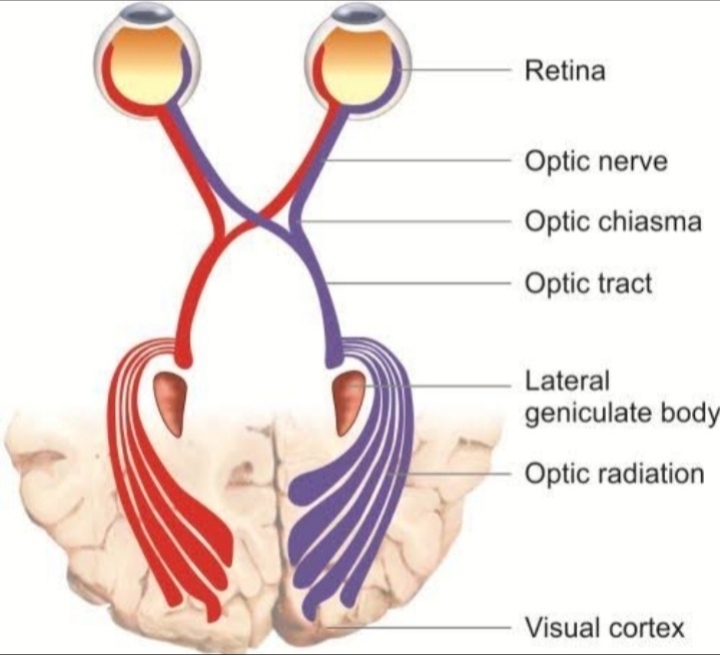
1.Sensory nerve supply comes from the lacrimal nerve, a branch of ophthalmic division of the fifth cranial nerve.
2.Sympathetic nerve supply comes from the carotid plexus of the cervical sympathetics.
3.Secretomotor fibres are derived from the superior salivary nucleus.
The accessory lacrimal glands
These include:
- Glands of Krause
- Glands of Wolfring
- Infraorbital glands
- Glands in the caruncle and plica semilunaris
- Glands of Krause : These are microscopic glands lying in the subconjunctival tissue of the fornices. These are about 40-42 in the upper fornix and about 6-8 in the lower fornix. Their ducts unite to form a long duct which open in the fornix.
- Glands of Wolfring: These are microscopic glands present along the upper border of superior tarsus (2-5 in numbers), and lower border of inferior tarsus (2-3 in numbers).
- Rudimentary accessory lacrimal glands : These are present in the caruncle , plica semilunaris and
Disease of Lacrimal Gland
- Acute dacryoadenitis:
- It usually accompanies a systemic disease like mumps, influenza or glandular fever.
- It is characterized by acute local pain, swelling and tenderness and drooping of the outer part of the upper lid with a characteristic S- shaped curve.
- Treatment: The infection is usually self – limiting.
Antibiotics with local hot compress may be required in some cases.
- Chronic dacryoadenitis:
- A proliferative inflammation of the lacrimal gland, may occur as apart of generalized granulomatous disorders (e.g. syphilis, tuberculosis or sarcoidosis).
- It presents as a painless, firm, mobile swelling of the lacrimal glands.
- Treatment is directed towards the underlying cause.
Lacrimal glands tumours:
- They are relatively rare, and show a marked resemblance to the parotid gland tumours.
- They present in middle – aged, progressive slowly, until they become palpable as hard, nodular and slightly mobile lumps.
- Proptosis occurs in downwards and medially, along with limitation of movements and diplopia.
- Benign mixed tumours form the majority and have an excellent prognosis if they are excised completely with their capsule.
- Carcinomas have a more rapid onset, often with pain and lymph node involvement. Local hyperostosis of the orbital bone is often evident on X- ray.
Treatment: A biopsy may be needed to confirm the diagnosis. If malignant, a radical surgical removal or a full exenteration of the orbit is often advisable.