Objectives –
- Anatomy and course of occulosympathetic pathway
- Horners syndrome
- What is Horners Syndrome
- Causes of Horners Syndrome
Anatomy and course of occulosympathetic pathway:
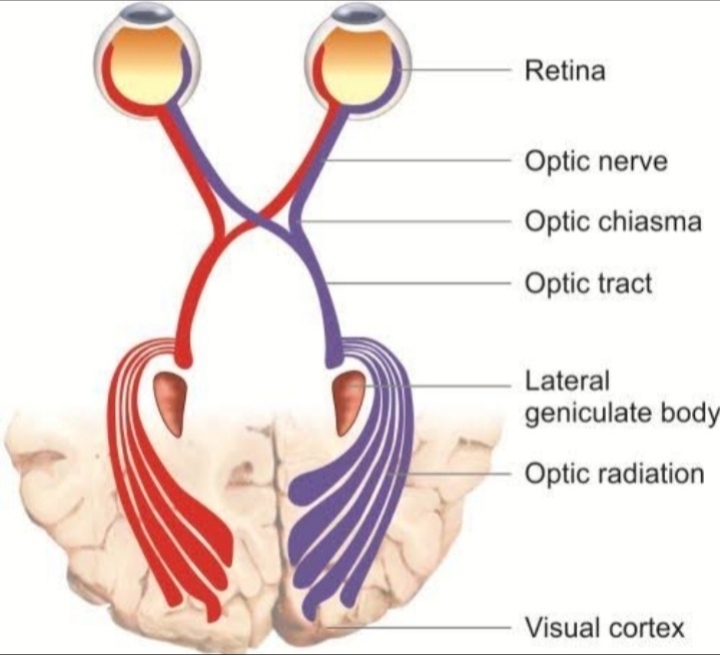
The sympathetic nerve supply to the whole body comes from a special structure called hypothalamus . It is sheet of grey matter which is present inside the central nervous system just above the pituitary gland . The sympathetic down going fiber they goes down along a special pathway called poly neuronal pathway ,and they goes laterally down the central nervous system , and it emerges out from the thoraco lumbar region of the spinal cord . The sympathetic inervation to the head and neck goes out from C-5(cervical ), T-2(thoracic) , T-8 region of the spinal cord , from a special place called cilio spinal center of budge . After emerging out from the spinal cord they enter into the middle cervical ganglion and they do not relay there . Some fibers from there goes to the superior cervical ganglion , and some goes to the inferior cervical ganglion and forms a para vertibral chain .
From the superior cervical ganglion post ganglionic sympathetic fibers arises and they enter into the internal carotid artery and forms a plexus around it and as the internal carotid artery enters the cavernous sinus , some sympathetic fibers goes with the superior part of the occulomotor nerve and supply the muscle of Muller . Also some fibers from the internal carotid artery jumps and goes with the nasociliary nerve of the opthalmic division and enters into the eye and Supply the dilator pupili. Where as some fibers goes with external carotid artery and supply the vasomotor and sudomotor fibers of the head and neck .
Horners syndrome
- What is Horners Syndrome?
- It is a clinical manifestations where the sympathetic inervation to the head and neck is completely lost. As the function of dilator pupili is partially lost , the patient will have constricted pupil with partial ptosis . It often occurs unilaterally where the sudomotor fibers also lost it’s function and patient may develop Anhidrosis ( no sweating ) or hypohidrosis (reduced sweating ) . As it occurs unilaterally there may be also pupil size difference , the condition is called anisocoria .
2. Causes of Horners syndrome
There are many causes of Horners Syndrome
First order neuron damage
- Neoplastic infiltration
- Infraction
- Demyelination
- Malformations
- Degeneration
- Neoplastic infiltration – Any overgrowth or tumour in CNS , such as pituitary apoplexy where the blood vessels inside the pituitary gland overgrow and irretate and damage the occulosympathetic pathway and produce Horners Syndrome .
- Infraction – if there is sudden Aschemia or sudden reduction in blood flow to the CNS, then lateral medullary syndrome or lateral Pontine syndrome can occur . The lateral medullary syndrome also has a special name called wallen berg syndrome . Here the posterior inferior cerebellar artery is damaged along with lateral downgoing sympathetic fibers . So the person may develop ataxia , nystagmus , vertigo along with Horners Syndrome .
- Demyelination – CNS disease such as multiple sclerosis can damage the sympathetic down going fibers and may produce Horners Syndrome .
- Malformations – disease such as Arnold chiari malformations , where due to some problems in the superior cranial fossa the cerebellar tonsils goes down and push through the foramen Magnum and damage the outgoing the sympathetic nerve fibres .
- Degeneration – disease of spinal cord such as syringo mylea , where the dorsal rhemus and the ventral rhemus undergoes infraction and spinal canal grows excessively and damages the sympathetic nerve fibres and causes Horners syndrome .
Second order neuron damage
- Small cell carcinoma at the top of the lung – also known as pancoast tumour , where the sympathetic para vertibral chain is involved along with brachial plexus where it produce pain in the hand , it irritate the phrenic nerve and produce hiccups , it also irritate the recurrent laryngial nerve and produce horness of voice .
- Lymphadenopathy , sarcoidosis , tuberclorosis can also involves the outgoing sympathetic fibers .
- Central venous catheterization can also lead to damage to the sympathetic fibers .
Other causes of Horners syndrome
- In diabetic mother the size of the baby is usually larger , so when the mother is giving a natural birth , and if the baby’s brachial plexus is damaged during the head pull it may cause damage to sympathetic fibers
- The colour of iris is maintained by a pigment called melatonin depends mainly on the sympathetic inervation and if it is damaged the colour of the iris degrade and causes a condition called heterochromia .
- Any Infection in cavernous sinus such as cavernous sinus thrombosis , carotido cavernous fistula can also cause Horners syndrome .
- A virus called herpes zoster can also damage the sympathetic fibers and causes Horners syndrome .
- Internal carotid artery dissection – here a gush of blood leaks out from the wall of the lumen and goes around the adventitia and causes hammreoge .