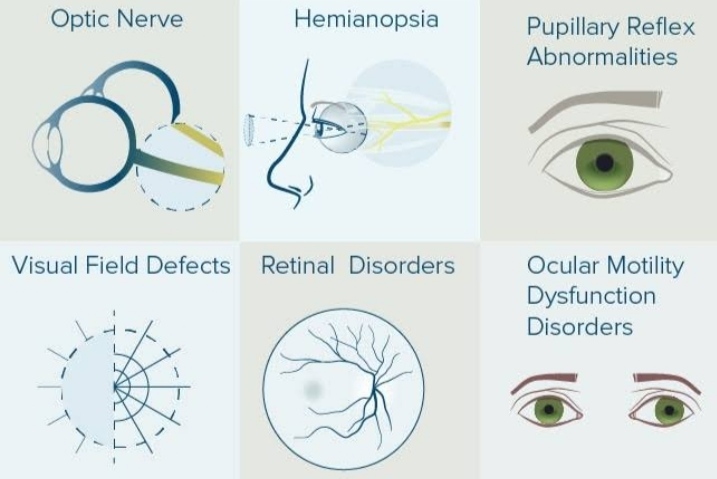
Ocular related disease of the central nervous system is not infrequent. There are many disease known to cause ocular or visual changes. A few common lesions of these diseases are discussed here.
•Intracranial infection:
These include meningitis, encephalitis, brain abscess and neurosyphilis.
- Meningitis:-
It may be complicated by paralysis of third, fourth, and sixth cranial nerves and papillitis. Chronic chiasmal arachnoditis may produce bilateral optic atrophy. Tuberculosis meningitis may be associated with choroidial tubercles. - Encephalitis:-
It may be complicated by papillitis Or papilloedema. Cranial nerve palsies are usually incomplete. Ptosis and diplopia are often present. - Brain abscess:-
It is frequently connected with papilloedema. Focal signs depend upon the site of the abscess and are thus similar to tumours. - Neurosyphilis:-
Ocular involvement is quite frequent. Gummatous meningitis may be associated with papillitis, papilloedema or postneuritic optic atrophy and cranial nerve palsies. Third cranial nerve is paralyzed in nearly 30% cases, less frequently the fifth and sixth, and least frequently the fourth. Tabes dorsalis and generalised paralysis of insane may be associated with primary optic atrophy, argyll Robertson pupil and internal and external ophthalmoplegia.
•intracranial aneurysm:
Intracranial aneurysms associated with ocular manifestation are located around the circle of willis. Intracranial aneurysms may produce complications by following mechanisms:
1.production of arteriolar venous fistula:-
carotid carvernous fistula may be produce by rupture of a giant aneurysm of the intracavenous part of the internal carotid artery. Pulsating exophthalmos is a typical presentation of carotid carvenous fistula.
- Pressure effects are as follows:
i. Aneurysms of circle of willis and internal carotid artery (supraclinoid, infraclinoid, intracavenous, and anterior communicating artery) may produce following pressure effects:
•Slowly progressive ophthalmoplegia, due to pressure, on motor nerves in the carvenous sinus.
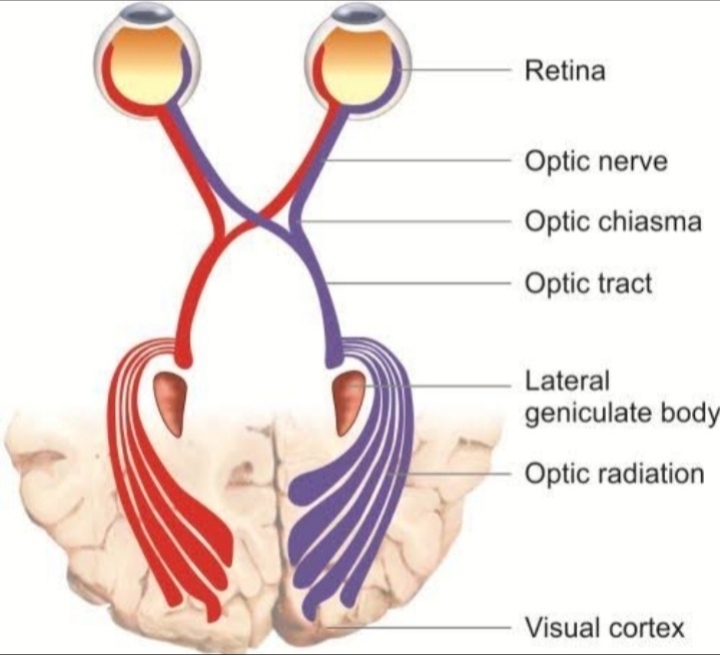
•central and peripheral visual loss due to pressure on intracranial part of optic nerve and chiasma.
•horner’s syndrome due to pressure on sympathetic fibres along the carotid artery.
It is due to disturbance of the sympathetic nerve supply to the dilator pupillae muscle. The sympathetic pathway starts from the posterior hypothalamus. The descending fibres reach the cilio spinal centre of budge in the spinal cord. From here, the fibres travel to the superior cervical ganglion in the neck. The post ganglionic fibres join the ophthalmic branch of trigeminal nerve and reach the dilator pupillae via the long ciliary nerves. Along with the dilator pupillae, these nerves also supply the muller’s muscle of the lids and the sweat gland.
•facial pain and paraesthesia associated with corneal anaesthesia due to pressure on the branches of trigeminal nerve.
ii. Vertebrobasilar artery aneurysms may also be associated with third nerve palsy.
iii. Posterior communicating artery aneurysm typically present with isolated painful third nerve palsy. - Subarachonoid haemorrhage:- subarachonoid haemorrhage is a life threatening complication associated with sudden rupture of aneurysm of the circle of willis. It is characterized by:
•third nerve palsy with pupillary dilatation.
•sudden violent headache.
•photophobia signs of meningeal irritation, vomiting and unconsciousness.
•terson syndrome refers to the combination of bilateral intraocular haemorrhage and subarachonoid haemorrhage due to aneurysmal rupture.
•intracranial hemorrhages:
Ophthalmic signs of subarachonoid haemorrhage may produce retinal haemorrhages, papilloedema and ocular palsies. Intracerebral haemorrhage are tonic conjugate and dysconjugate deviations.
•intracranial space occupying lesions(ICSOLs) :
These include primary and secondary brain tumours, granulomatous inflammation, haematomas, and parasitic cysts. Clinical features of the ICSOLs may be described under three heads:
I. General effects of raised intracranial pressure:- these include headache, papilloedema, vomiting, drowsiness, giddiness, slowing of pulse rate and rise in blood pressure.
II. False localising signs:- these occur due to the effect of raised intracranial pressure and displacement or distortion of the brain tissue. False localising signs of ophthalmological interest are as follows:
- Bitemporal hemianopia: it results from downward pressure of the distended third ventricle on the chiasma.
- Diplopia: it occurs due to pressure palsy of the sixth nerve.
- Homonymous hemianopia: it may result from occipital herniation through the tentorium cerebelli with compression of the posterior cerebral artery.
- Sluggish pupillary reflexes and unilateral mydriasis: may occur due to pressure on the third nerve.
III. Focal signs of intracranial mass lesions:- these depend upon the site of the lesions. Focal signs of ophthalmological interest are as follows:
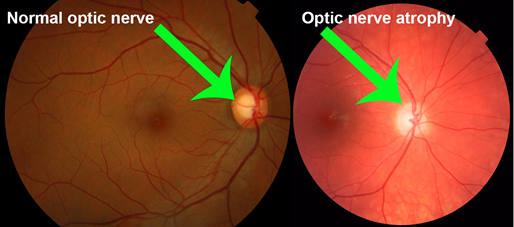
- Prefrontal tumours: particularly meningioma of the olfactory groove, are associated with a pressure atrophy of the optic nerve on the side of lesions and papilloedema on the other side due to raised intracranial pressure.
- Temporal love tumours: these may produce incongruous crossed upper quadrantanopia due to pressure on the optic radiations. Visual hallucinations may occur owing to irritation of the visuo-psychic area. Third and fifth cranial nerves may be involved due to downward pressure. Impairment of convergence and of superior conjugate movements may occur in late stages due to prolapse of the uncus through the tentorium cerebelli into the posterior fossa, with resulting distortion of the ventral part of midbrain.
- Parietal lobe tumours: these are associated with crossed lower homonymous quadrantanopia due to involvement of the upper fibres of the optic radiations. Other lesions include visual and auditory hallucinations, conjugate deviation of the eyes and optokinetic nystagmus.
- Occipital lobe tumours: these may produce crossed homonymous quadrantic Or hemianopic defect involving the fixation point. Visual agnosia may also be associated.
- Midbrain tumours: these may be associated with homonymous hemianopia due to pressure on the optic tracts. Other signs depending upon the site of involvement are as follows:
i. Tumours of the upper part produce spasmodic contraction of the upper lid followed by ptosis and loss of upward conjugate movements. In about 25% cases, an upper motor neuron facial paralysis and ipsilateral hemiplegia may also develop.
ii. Tumours of the intermediate level may be associated with the following syndromes: (i) Weber’s syndrome, it is characterized by ipsilateral third nerve palsy, contralateral hemiplegia and facial palsy of upper motor neuron type. (ii) Benedict’s syndrome, it is characterized by ipsilateral third nerve palsy associated with tremors and jerky movements of the contralateral side which occur due to involvement of the red nucleus. - Tumours of the pons: lesions in the upper part are characterized by ipsilateral third nerve palsy, contralateral hemiplegia and upper motor neuron type facial palsy. While the lesions in the lower part of the pons produce Mallard-Gubler syndrome which consists of ipsilateral sixth nerve palsy, contralateral hemiplegia and ipsilateral facial palsy or foville’s syndrome in which sixth nerve paralysis is replaced by loss of conjugate movements to the same side.
7.cerebellar tumours: those arising from the cerebellopontine angle produce corneal anaesthesia due to involvement of fifth nerve, early deafness and tinnitis of one side, sixth and seventh cranial nerve paralysis, cerebellar symptoms such as ataxia and vertigo, marked papilloedema and nystagmus. - Chiasmal and pituitary tumours: these include pituitary adenomas craniopharyngiomas and suprasellar meningiomas. These tumours typically produce chiasmal syndrome which is characterized by bitemporal visual field defects, optic atrophy and sometimes endocrinal disturbances.
•Demyelinating diseases:
These include multiple sclerosis, diffuse sclerosis, and neuromyelitis optica(Devic’s disease). Ocular involvement may occur in all these conditions. Their salient features are as follows:
Multiple sclerosis or demyelination:- optic neuritis is the presenting feature in about 25% of multiple sclerosis patient, and in 70% cases, it occurs in established disease. Recurrence in the same eye or opposite eye occurs in about 25% patient. The impairment of vision is more with increased body temperature (uhthoff’s phenomenon).
Diffuse sclerosis (schilder’s disease) :- it typically affects children and adolescents and is characterized by progressive demyelination of the entire white matter of the cerebral hemispheres. Ocular lesions include: optic neuritis, cortical blindness, ophthalmoplegia and nystagmus.
Neuromyelitis optica (of devic): it is characterized by bilateral optic neuritis associated with ascending myelitis, entailing a progressive quadriplegic and anaesthesia. Unlike multiple sclerosis, this condition is not characterised by remissions and is not associated with ocular palsies and nystagmus.
•ocular signs in head injury:
Ocular signs related only to the intracranial damage are describe here. However direct trauma to the eyeball and Or orbit is frequently associated with the head injury.
A. Concussion injuries to the brain:- there are usually associated with subdural haemorrhage and unconsciousness which may produce the following ocular signs:
- Papilloedema: papilloedema is the bilateral, noninflammatory passive swelling of the optic disc, produced by raised intracranial tension (ICT).
• papilloedema is one of the causes of disc edema, and they are not synonymous.
•generally unilateral causes of disc edema should be considered to be due to a local inflammation, vascular disorders, or compressive lesions in the orbit.
• unilateral papilloedema with optic atrophy on the other side suggests a frontal lobe tumor or olfactory meningioma of the opposite side the Foster Kennedy syndrome.
•as a rule, papilloedema does not develop if the optic nerve has already become atrophic.
- Hutchinson’s pupil: it is characterised by initial ipsilateral miosis followed by dilatation with no light reflex due to raised intracranial pressure. If the pressure rises still further, similar changes occur in the contralateral pupil. Therefore presence of bilateral fixed and dilated pupils is an indication of immediate cerebral decompression.
B. Fractures of the base of skull:- associated ocular signs are as follows:
- Optic nerve injury:- it may be injured directly indirectly or compressed by the haemorrhage. Primary optic atrophy may appear in 2-4 weeks following injury. Presence of papilloedema suggests haemorrhage into the nerve sheath.
- Cranial nerve palsies:- there are often seen with fractures of the base of the skull most common being the ipsilateral facial paralysis of the lower motor neuron type. Extraocular muscle palsies due to involvement of sixth, third and fourth cranial nerves may also be seen.
- Pupillary signs:- these are inconsistent and thus not pathognomonic. However usually pupil is dilated on the affected side.
- Subconjunctival haemorrhage:- it may be seen when fracture of the base of skull is associated with fractures of orbital roof. The subconjunctival haemorrhage is usually more marked in the upper quadrant and ite posterior limit cannot be reached.