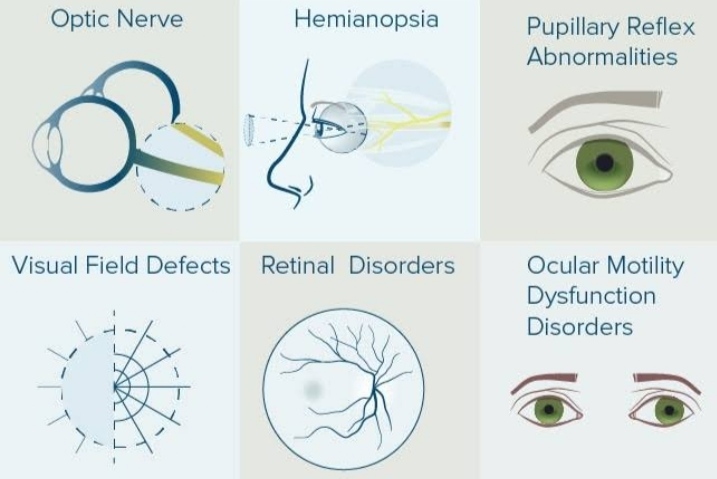
Pupillary light reflex is used to assess the brain stem function. Abnormal pupillary light reflex can be found in optic nerve injury, oculomotor nerve damage, brain stem lesions, such as tumors, and medications like barbiturates.
Pupillary abnormalities
Pupillary disorders may involve the afferent pathways (RAPD) or the efferent pathways. Anisocoria, where not physiological, indicates a problem of the efferent pupillary pathway, either parasympathetic or sympathetic (Horner’s syndrome). Disorders of the parasympathetic system impair the light response and they include third nerve palsy and tonic pupil. Disorders of the iris, including application of cholinergic agents, also need to be considered in impaired pupillary light reaction.
Anisocoria
This refers to unequal pupils. Anisocoria is physiological (and harmless) in about 20% of people. Anisocoria of new onset can suggest serious underlying pathology such as trauma, Horner’s syndrome, pharmacological mydriasis/miosis, or third nerve palsy.
It is necessary to ascertain first which pupil is behaving abnormally. Compare the pupils in light and dim conditions:
Unilateral large pupil
This is a pupil showing poor constriction in a well-lit room. Causes include:
- Traumatic iris damage.
- Third cranial nerve palsy.
- Rubeosis iridis (neovascular eye disease).
- Holmes-Adie syndrome: may also be irregular, unusually unilateral – see below.
- Pharmacological dilation (ie dilating drops).
Unilateral small pupil
This is a pupil showing poor dilatation in low light. Causes include:
- Physiologically small pupil.
- Uveitis with synaechiae.
- Horner’s syndrome.
- Argyll Robertson (AR) pupil (may also be irregular, usually bilateral – see below).
- Pharmacological constriction (constricting drops).
Impaired pupillary light reflex
Normally, pupils react (ie constrict) equally. Comparing the direct and consensual reaction to light in both eyes is helpful in locating a lesion, remembering that the retina and optic nerve are needed for the afferent signal and that the oculomotor nerve provides the efferent component of both the direct and consensual reflexes.
Relative afferent pupillary defect
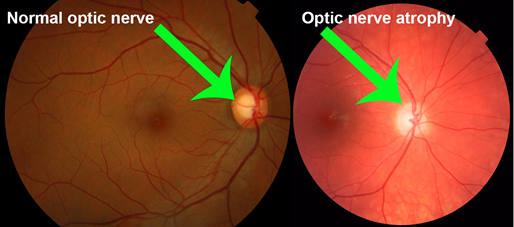
An RAPD is a defect in the direct pupillary response and usually suggests optic nerve disease or severe retinal disease. Causes include:
- Unilateral optic neuropathies are common causes of an RAPD. These include arteritic (giant cell arteritis) and non-arteritic causes. Usually there will be a loss of vision or of part the visual field.
- Optic neuritis: even very mild optic neuritis can lead to a very strong RAPD.
- Severe glaucoma: while glaucoma normally is a bilateral disease, if one optic nerve has particularly severe damage, an RAPD can be seen.
- Traumatic optic neuropathy: this includes direct ocular trauma, orbital trauma, and head injuries which damage the optic nerve as it passes through the optic canal.
- Optic nerve tumour: this is a rare cause.
- Orbital disease: including compressive damage to the optic nerve from thyroid-related orbitopathy, orbital tumours, or vascular malformations.
- Optic atrophy: such as Leber’s optic atrophy.
- Optic nerve infections or inflammations: cryptococcus can cause severe optic nerve infection in the immunocompromised. Sarcoidosis can cause inflammation of the optic nerve. Lyme disease can affect the optic nerve.
- Severe ischaemic retinal disease – eg, ischaemic central retinal vein occlusion, central retinal artery occlusion, sickle-cell retinopathy.
- Retinal detachment: an RAPD can often be seen if the macula is detached.
- Very severe unilateral macular degeneration.
- Amblyopia
Non-reactive pupil
A unilateral fixed dilated pupil suggests injury or compression of the third cranial nerve and the upper brain stem. Fixed and dilated pupils in comatose patients indicate a poor prognosis, especially when present bilaterally.

Causes of a unilateral non-reactive pupil
- Post-traumatic iridocyclitis – eg, direct facial trauma.
- Serious intracranial pathology – eg, extending intracranial mass, intracranial haemorrhage, subarachnoid haemorrhage.
- Diffuse brain injury.
- Oculomotor nerve (CN III) palsy (see below).
- A large poorly reactive pupil with diplopia is the most common presentation of an aneurysm of the posterior communicating artery.
- Pharmacological (anticholinergic) blockade.
- Ocular prosthesis: the normal pupil may be relatively constricted.
Causes of bilateral non-reactive pupils
- Extensive intracranial pathology – eg, trauma, haemorrhage.
- Diffuse brain injury.
- Brain stem herniation, brain death.
- Pharmacological blockade.
Third cranial nerve palsy
When the pupil is involved in a oculomotor nerve palsy, it is fixed and dilated (or minimally reactive). A partially dilated pupil which reacts sluggishly to light suggests a relative pupil-sparing CN III palsy.
CN III palsy with involvement of pupil requires urgent investigation. Relative pupil-sparing CN III palsy is usually ischaemic in nature and is less urgent unless there is progression.
Horner’s syndrome
This is a relatively rare disorder caused by an interruption of the sympathetic nerve supply to the eye. The classic signs are:
- A constricted pupil.
- Ptosis.
- Absence of facial sweating (anhidrosis).
- Enophthalmos.
Near-light dissociation pupils
Holmes-Adie pupil (Adie’s tonic pupil)
- This most commonly affects younger women (3rd/4th decade).
- The condition is benign.
- The pupil is dilated in the early stages and may also be irregular.
- The pupil reacts slowly to light but briskly to accommodation (ie light-near dissociation).
- Once the pupil has constricted it remains small for an abnormally long time (tonic pupil).
- 80% are unilateral.
Argyll Robertson (AR) pupil
- This is usually bilateral (although it can be asymmetrical).
- A tonically small pupil that reacts poorly or not at all to light but briskly to accommodation (light-near dissociation).
- The pupils are difficult to pharmacologically dilate.
- Believed to be due to bilateral damage to nuclei in the midbrain.
- Considered highly specific for neurosyphilis, the most common cause.
- Other, very rare causes include:
- Diabetic neuropathy.
- Alcoholic midbrain degeneration.
- Parinaud’s dorsal midbrain syndrome: this is caused by a tumour of the pineal gland, which impairs vertical gaze and causes pseudo-AR pupils.
- Encephalitis.
- Amyloidosis.
- Multiple sclerosis.
- Midbrain tumours.