Introduction –
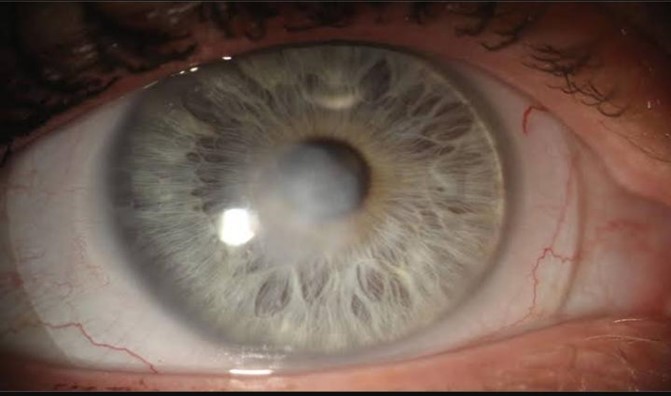
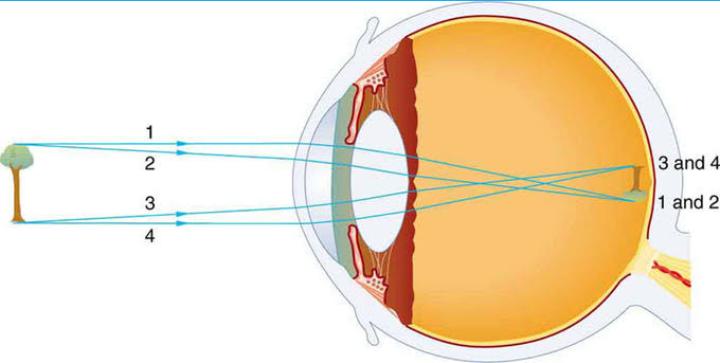
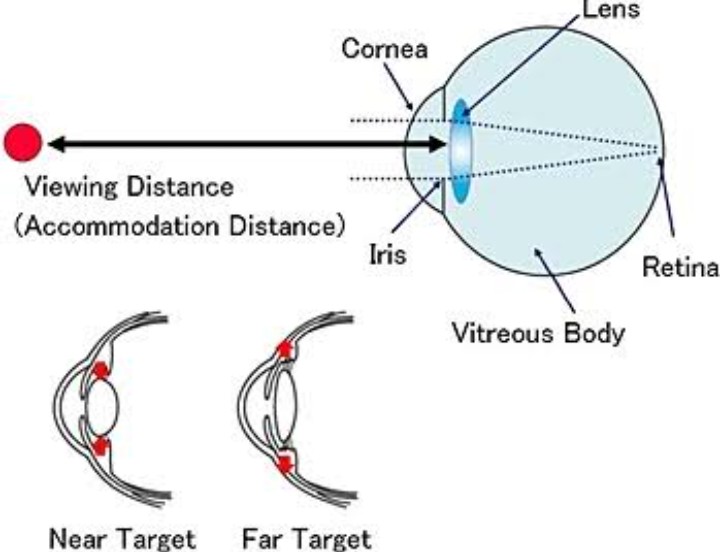
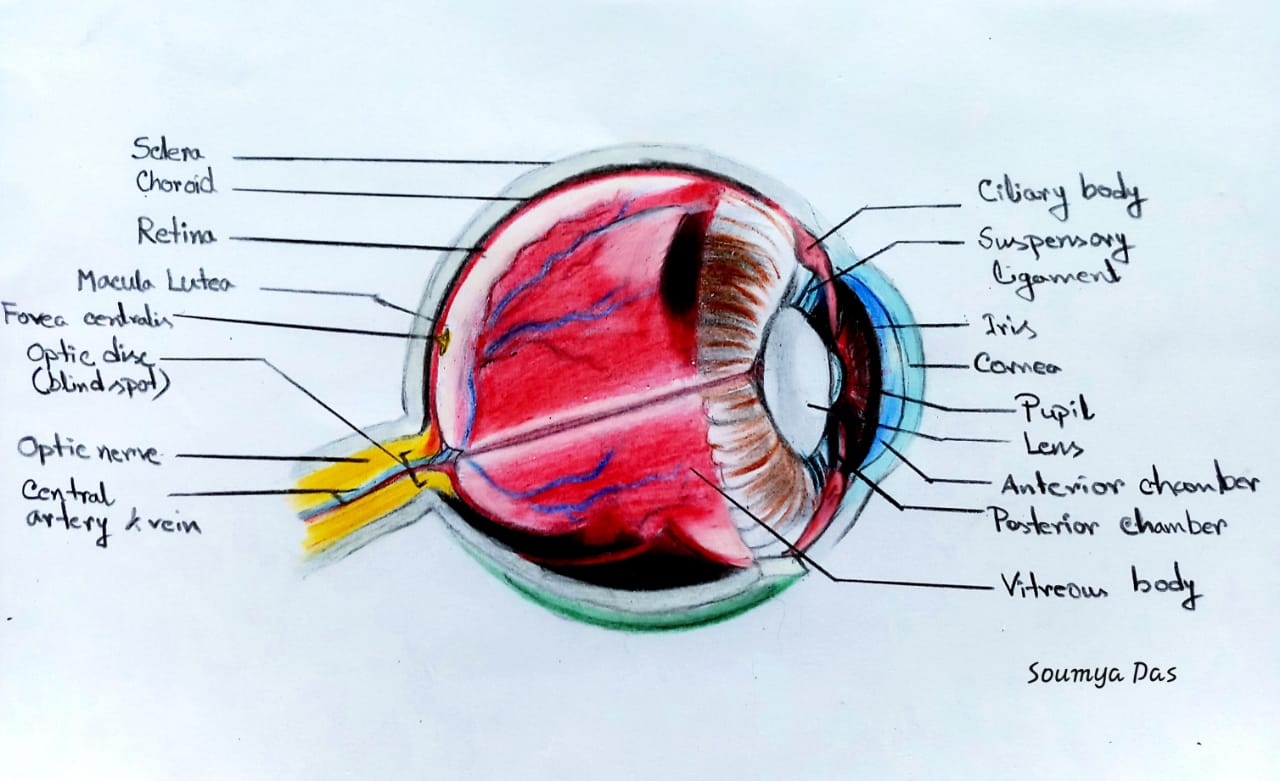
The human eye is a complex organ of vital importance for everyday life. Eyes are the parts of our body that perceive light to see the world and to understand how objects relate to each other. We can distinguish far objects from close ones and determine their color and shape. The cornea is the dome-shaped window in the front of the eye. When looking at a person’s eye, one can see the iris and pupil through the normally clear cornea. The cornea bends light rays as a result of its curved shape and accounts for approximately two-thirds of the eyes total optical power, with the lens of the eye contributing the remaining one-third. The cornea is as smooth and clear as glass but is strong and durable. It helps to shield the rest of the eye from germs, dust, and other harmful matter. The cornea shares this protective task with the eyelids, the eye socket, tears, and the sclera, or white part of the eye. A very thin tear film lies between the front of the cornea and our environment. The cornea copes very well with minor injuries or abrasions. If the highly sensitive cornea is scratched, healthy cells slide over quickly and patch the injury before infection occurs and vision is affected. Bacterial keratitis is an infection and inflammation of the cornea that cause pain, reduced vision, light sensitivity and tearing or discharge from the eye that can, in severe cases cause loss of vision. Bacterial keratitis progresses rapidly and corneal destruction may be complete in 24 – 48 hours with some of the more virulent bacteria. The
severity of the corneal infection usually depends on the underlying condition of the cornea and the pathogenicity of the infecting bacteria. It may involve the center of the cornea or the peripheral part of the cornea (that portion closest to the sclera) or both. Keratitis may affect one eye or both eyes. Keratitis may be mild, moderate, or severe and may be associated with inflammation of other parts of the eye. Keratitis can be classified by its location, severity, and cause. If keratitis involves the surface (epithelial) layer of the cornea, it is called superficial keratitis. Kerato-conjunctivitis is inflammation of the cornea and the conjunctiva. Kerato- uveitis is inflammation of the cornea and the uveal tract, which consists of the iris, ciliary body, and choroid. Keratitis may be acute or chronic. It may occur only once or twice in an eye or be recurrent. It may be limited in its effects on the eye or be progressive in its damage. Bacterial keratitis is a sight-threatening process. Many patients have a poor clinical outcome if aggressive and appropriate therapy is not promptly initiated. Some cases of keratitis results from unknown factors. Until recently, most cases of bacterial keratitis were associated with ocular trauma or
ocular surface diseases. Various types of infections, dry eyes, injury, and a large variety of
underlying medical diseases may all lead to keratitis. Dry eye syndrome (DES; keratoconjunctivitis
sicca) is a disorder of the tear film due to tear deficiency or excessive evaporation, which cause damage
to the ocular surface. The signs of DES include foreign body sensation, ocular discomfort (scratchy, dry,
sore, gritty, burning sensations) and problems with visual acuity. Bacterial keratitis accounts for approximately 65% to 90% of all corneal infections. The spectrum of bacterial keratitis can also be influenced by geographic and climatic factors. Many differences in keratitis profile have been noted between populations living in rural or in city areas, in western, or in developing countries. Ulcerations of the cornea may occur, a condition known as ulcerative keratitis. Before the advent of antibiotics, syphilis was a frequent cause of keratitis. Corneal ulceration, stromal abscess formation, surrounding corneal edema, and anterior segment inflammation are characteristic of this disease. There are several types of keratitis, including superficial punctate keratitis, in which the cells on the surface of the cornea die; interstitial keratitis, a condition that can be either the direct result of infection, or more commonly secondary to an immunologic process; herpes simplex viral keratitis, caused by the sexually transmitted herpes virus; and traumatic keratitis, which results when a corneal injury leaves scar tissue. Early diagnosis and treatment is the key to minimizing any visual-threatening sequelae. In addition, close follow-up, attention to laboratory data, and changing antimicrobials if no clinical improvement is evident are important elements for successful outcome. The severity of the corneal infection usually depends on the underlying condition of the cornea and the pathogenicity of the infecting bacteria. Many patients have a poor clinical outcome if aggressive and appropriate therapy is not promptly initiated.
Causes of bacterial keratitis –
Keratitis can lead to vision loss from corneal scarring. Physical or chemical trauma is a frequent cause of
keratitis. If the cornea is hit and damaged by a foreign body (a finger nail, an arm, a metal splinter or
through contact lenses), can cause a scratch to the cornea. Scratches are usually harmless and not very
deep, but they give bacteria and viruses the possibility of attacks, which gives the cornea inflammation
and should therefore be detected and treated. There are various types of keratitis, but most commonly it
occurs after an injury to the cornea, dryness, inflammation of the ocular surface or contact lens wear. A
wide variety of conditions can lead to inflammation of the cornea. Among them are viral, bacterial, or
fungal infections; exposure to ultraviolet light such as sunlight or sunlamps; exposure to other intense
light sources such as welding arcs or snow or water reflections; irritation from excessive use of contact
lenses; dry eyes caused by an eyelid disorder or insufficient tear formation; a foreign object in the eye; a
vitamin A deficiency; or a reaction to eye drops, eye cosmetics, pollution, or airborne particles such as
dust, pollen, mold, or yeast. The condition is also a side effect of certain medications. Bacterial keratitis
remains one of the most important potential complications of contact lens use and refractive corneal
surgery. Organisms can infiltrate an intact cornea of a lens-wearer, and a biofilm can form on the contact
lens. Interruption of an intact corneal epithelium and/or abnormal tear film permits entrance of
microorganisms into the corneal stroma, where they may proliferate and cause ulceration or secondary
effect or molecules and cause infection. The epithelium and stroma in the area of injury and infection
swell and undergo necrosis. Acute inflammatory cells (mainly neutrophils) surround the beginning ulcer
and cause necrosis of the stromal lamellae. The collagen of the corneal stroma is poorly tolerant of the
bacterial and leukocytic enzymes, and undergoes degradation, necrosis and thinning. This leads to
scarring of the cornea. As thinning advances, the cornea may perforate, thus introducing bacteria into the
eye with ensuing endophthalmitis. Corneal infections rarely occur in the normal eye. They are a result of
an alteration in the comea's defense mechanisms that allow bacteria to invade when an epithelial defect is
present. The organisms may come from the tear film or as a contaminant from foreign bodies, contact
lenses or irrigating solutions. The severity of the disease depends on the strain of the organism, the size
of the inoculums, the susceptibility of the host and immune response, the antecedent therapy and the
duration of the infection. The process of corneal destruction can take place rapidly (within 24hrs with
virulent organisms) so that rapid recognition and initiation of treatment is imperative to prevent visual loss.
Contact lens users are at an increased risk of corneal ulcers . The annual incidence of bacterial keratitis
with daily-wear lenses is 3 cases per 10,000. Contact lens is the leading cause of corneal inflammation,
and if we as a contact lens user experience the following symptoms should seek medical attention right
away. The injury may become secondarily infected or remain noninfectious. Retained corneal foreign
bodies are frequent sources of keratitis.
Complications with keratitis –
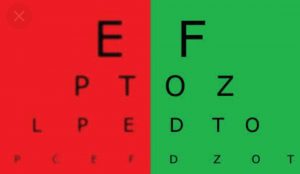
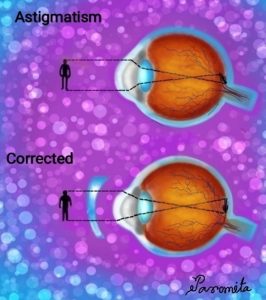
Irregular astigmatism: Another possible complication of these infections is uneven healing of the stroma,
resulting in irregular astigmatism.
Corneal perforation: This is one of the most feared complications of bacterial keratitis that may result in secondary endophthalmitis and possible loss of the eye.
Treatment –
Medical treatment is absolutely essential – even a delay of a few hours can affect the ultimate visual
result. The causative factors must be determined through laboratory analysis of scrapings; medical
treatment (i.e., medication) varies according to the cause. As with bacterial conjunctivitis, culturing the
infection is the ideal way to determine the infecting organism but is often difficult or impractical. First and foremost, you must halt bacterial proliferation; do not delay treatment while waiting for the culture results.
If you have the materials available, scrape the ulcer using a platinum spatula and plate the specimen into
blood and chocolate agar culture media. A simpler but less effective method is to use a
culturette, Regardless, immediately begin therapy with a broad spectrum antibiotic. A popular initial
therapy is the fluoroquinolone ciprofloxacin 0.3% (Ciloxan) two drops every 15 minutes for six hours,
followed by two drops every 30 minutes for 18 hours, and then tapered depending on patient response.
Infectious keratitis generally requires antibacterial therapy to treat the infection. This treatment can
involve prescription eye drops, pills, or even intravenous therapy. Any corneal or conjunctival foreign body should be removed. Wetting drops may be used if disturbance of the tears is suspected to be the cause of the keratitis. Steroid drops may often be prescribed to reduce inflammation and limit scarring. This must be done carefully and judiciously, since some infections can be worsened with their use. Treatment depends largely on the source of the problem. If a common adenoviral virus is causing the keratitis, the condition is likely to clear up on its own, usually in about two to three weeks. Available medications for this form of keratitis include palliative treatment. Contact-lens wearers are typically advised to discontinue contact-lens wear, whether or not the lenses are related to the cause of the keratitis.