Introduction:
The eye is the primary organ of vision. Each one of the two eyeballs is located in the orbit, where it takes up about one-fifth of the orbital volume. The remaining space is taken up by the extraocular muscles, fascia, fat, blood vessels, nerves and the lacrimal gland. The eye is embryologically an extension of the central nervous system. It shares many common anatomical and physiological properties with the brain. Both are protected by bony walls, have firm fibrous coverings and a dual blood supply to the essential nervous layer in the retina. The eye and brain have internal cavities perfused by fluids of like composition and under equivalent pressures. As the retina and optic nerve are outgrowths from the brain, it is not surprising that similar disease processes affect the eye and central nervous system. The physician should constantly remind himself or herself of the many disease conditions that can simultaneously involve the eye and the central nervous system.
Basic Structure of the Eye and Supporting Structures :
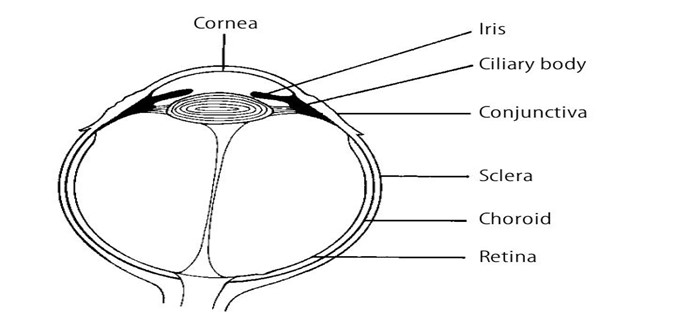
The eye has three layers or coats, three compartments and contains three fluids.
1. The three coats of the eye are as follows:
(a) Outer fibrous layer:
• cornea
• sclera
• lamina cribrosa.
(b) Middle vascular layer (uvula tract):
• iris
• ciliary body – consisting of the pars plicata and pars plana
• choroids.
(c) Inner nervous layer:
• pigment epithelium of the retina
• retinal photoreceptors
• retinal neurons
2. The three compartments of the eye are as follows:
(a) Anterior chamber : the space between the cornea and the iris diaphragm.
(b) Posterior chamber : the triangular space between the iris anteriorly, the lens and zonule posteriorly, and the ciliary body.
(c) Vitreous chamber : the space behind the lens and zonule.
3. The three intraocular fluids are as follows:
(a) Aqueous humor : a watery, optically clear solution of water and electrolytes similar to tissue fluids except that aqueous humor has a low protein content normally.
(b) Vitreous humor : a transparent gel consisting of a three-dimensional network of collagen fibers with the interspaces filled with polymerized hyaluronic acid molecules and water. It fills the space between the posterior surface of the lens, ciliary body and retina.
(c) Blood : in addition to its usual functions, blood contributes to the maintenance of intraocular pressure. Most of the blood within the eye is in the choroid. The choroidal blood flow represents the largest blood flow per unit tissue in the body. The degree of
desaturation of efferent choroidal blood is relatively small and indicates that the
choroidal vasculature has functions beyond retinal nutrition. It might be that the choroid serves as a heat exchanger for the retina, which absorbs energy as light strikes the retinal pigment epithelium. Clinically, the eye can be considered to be composed of two segments:
1. Anterior segment : all structures from (and including) the lens forward.
2. Posterior segment : all structures posterior to the lens.
The Outer Layer of the Eye :
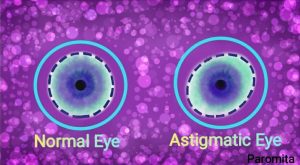
The anterior one-sixth of the fibrous layer of the eye is formed by the cornea. The
posterior five – sixths are formed by the sclera and lamina cribrosa. The cornea is
transparent, whereas the sclera, which is continuous within it, is white. The junction of cornea and sclera is known as the limbus. The cornea has five layers anteroposteriorly :
1. Epithelium and its basement membrane stratified squamous type of epithelium with five to six cell layers of regular arrangement.
2. Bowman’s layer : homogeneous sheet of modified stroma.
3. Stroma : consists of approximately 90% of total corneal thickness. Consists of
lamellae of collagen, cells and ground substance.
4. Descemet’s membrane : the basement membrane of the endothelium.
5. Endothelium : a single layer of cells lining the inner surface of Descemet’s
membrane.
In the region of the limbus, the epithelium on the outer surface of the cornea becomes continuous with that of the conjunctiva, a thin, loose transparent nonkeratinizing mucous membrane that covers the anterior part of the sclera, from which it is separated by loose connective tissue. Above and below, the conjunctiva is reflected onto the inner surface of the upper and lower lids. This mucous membrane, therefore, lines the posterior surface of the eyelids and there is a mucocutaneous junction on the lid margin. Although the conjunctiva is continuous, it can be divided descriptively into three parts: palpebral (tarsal), bulbar and fornix. The sclera consists of irregular lamellae of collagen fibers. Posteriorly, the external two thirds of the sclera become continuous with the dural sheath of the optic nerve, while the inner one-third becomes the lamina cribrosa – the fenestrated layer of dense collagen fibers through which the nerve fibers pass from the retina to the optic nerve. The sclera is thickest posteriorly and thinnest beneath the insertions of the recti muscles. There is a layer of loose connective tissue deep to the conjunctiva, overlying the sclera, called the episcleral.
Middle Layer:
The middle layer is highly vascular. If one were to peel the sclera away from this layer (not an easy task), the remaining structure would resemble a grape, as this middle layer, which is called the uvea, is heavily pigmented as well as being vascular. The anterior part of the uvea forms the bulk of the iris body and hence inflammation of the iris is called either anterior uveitis or iritis. The posterior part of the uvea is called the choroid. The iris is the most anterior part of the uvea. It is a thin circular disc perforated centrally by the pupil. Contraction of the iris sphincter muscle constricts the pupil, while contraction of the dilator pupillae muscle dilates the pupil. The ciliary body is part of the uveal tissue and is attached anteriorly to the iris and the scleral spur; posteriorly it is
continuous with the choroid and retina. The ciliary body is also referred to as the
intermediate uvea. The ciliary body is triangular in crosssection. The anterior side of the ciliary body is the shortest and borders the anterior chamber angle; it gives origin to the iris. The outer side of the triangle (mainly ciliary muscles) lies against the sclera. The inner side is divided into two zones: the pars plicata forms the anterior 2 mm and is covered by ciliary processes and the pars plana constitutes the posterior 4.5-mm flattened portion of the ciliary body. The pars plana is continuous with the choroid and retina. The choroid consists of the following:
• Bruch’s membrane – membrane on the
external surface of the retinal pigment epithelium (RPE). It consists of the basement
membrane of RPE cells and choriocapillaris. Between the two layers of basement
membrane are the elastic and collagenous layers. Small localized thickenings of
Bruch’s membrane (which increase with age) are called drusen.
• The choriocapillaris – a network of capillaries supplying the RPE and outer retina.
• Layer of larger choroidal blood vessels external to the choriocapillaris.
• Pigmented cells scattered in the choroid external to the choriocapillaris.
Inner layer:
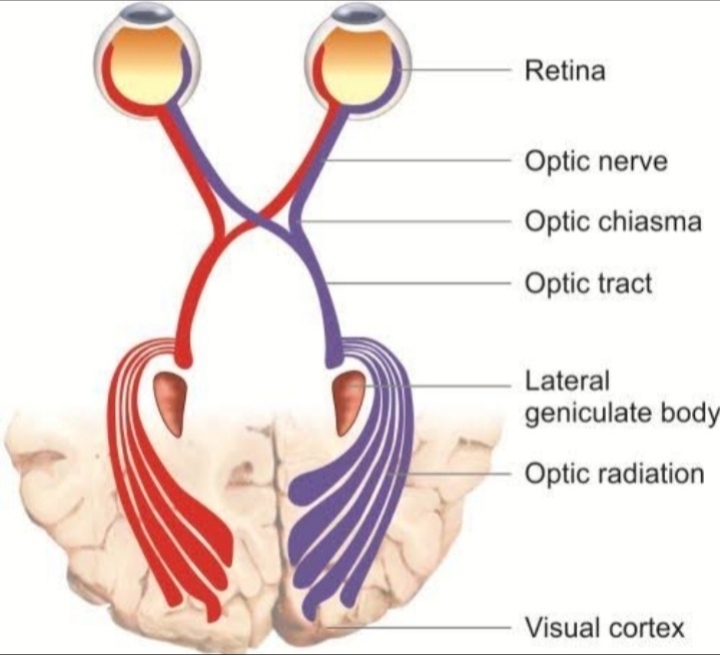
The inner layer of the eye, which lines the vascular uvea, is the neurosensory layer. This layer forms the retina posteriorly; but, anteriorly it comes to line the inner surface of the ciliary body and iris as a two-layered pigment epithelium. These same layers can be traced into the retina, which is composed of an outer pigment epithelium and an inner sensory part, which contains the rods and cones, bipolar cells and ganglion cells. The junction of the retina and the pars plana forms a scalloped border known as the ora serrata. It is important to note that the photoreceptor cells are on the external side of the sensory retina. The relationship of the retinal elements can be understood most readily by following the formation of the optic cup. As the single-cell layer optic vesicle “invaginates” to form the two cell layered optic cup, the initially superficial cells become
the inner layer of the cup. The RPE develops from the outer layer of the cup, facing the photoreceptors across the now obliterated cavity of the optic vesicle. The neurons of the sensory retina differentiate from the inner layer of the optic cup.