The value of tear flude of preserving a clear cornea has been understood sinces ages. The fact that the blinking action of lids was esentioal foe spreading the tears and maintaing a moist surface on anterior portion of globes was obvious even in olden age. Hence the knowledge of the precorneal liquid is of long- standing and so is the knowledge that the cornea will dry up, if tha blinking is prevented.
The pesence of precorneal layer of liquid was first demonstrated by Fischer in 1928by using light reflected from the corneal surface on a photographic plate.
Further studies showed it to be an important part of cornea and Rollet even described it as the most superficial, sixth layer of cornea.
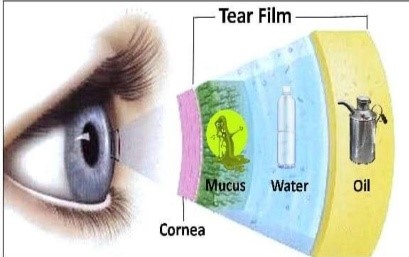
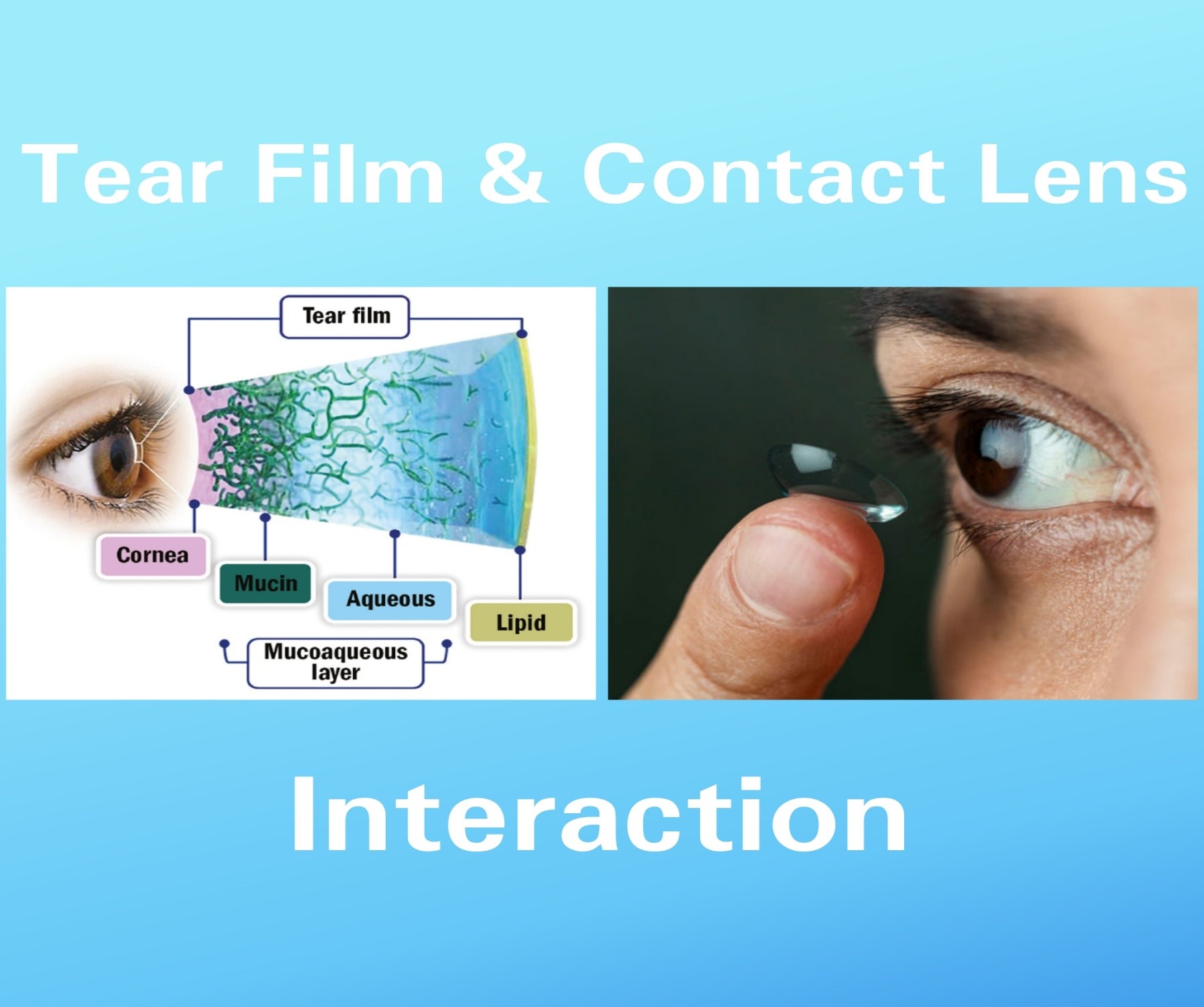
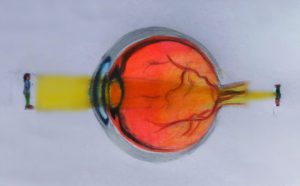
STRUCTURE OF TEAR FILM:
Wolf (1946) was the first to describe in detail the structure of tear film. He gave a clinical description of the fluid in the conjuctival sac with special reference to the lid margin. He coined the term “precorneal film” and assumed that it consisted of three layers, an outer oily layer, an intermidiated aqueous layer and an inner mucoid layer.
- LIPID LAYER:-
Outermost superficial oily layer to tear film derived from the secretions of Meibomian, Zeiss, and Moll glands covers the entire free surface of the tear fluid.
Marginal tear strip Wolf found that this layer, on the lid margins forms a strip which extends to the posterior margin of the openings of the meibomian glands and limits the anterior end of tear fluid reservations.
Physical intergrity of lipid layer: The thickness of lipid layer is about 0.1-0.2 mm and depends on the palpebral fissure width, i.e it incress when the lids are partially closed.
Control of lipid secretion is neuroendocrinal:
- Androgen sex hormones regulate lipid synthesis and secretion.
- Neurotransmitters from the nerves surrounding the acini can alter lipid synthesis or alveolar cell rupture.
Functions of lipid layer include: Oily layer of tear film prevents the overflow
of tears and retards their evaporation. The latter fact accrues from the observation that cauterization of the orifices of meibomian glands increases the evaporation by more than 10 times and results in absence of oily layer.
- It prevents migration of skin lipids onto the ocular surface.
- It provides a clear ocular medium and smooth surface for refraction of light.
- Acts as a barrier for preventing contamination of tear film.
- It acts as a surfactant layer which makes an effective bridge between the non-polar lipid phase and aqueous-mucinous phase.
It acts as a lubricant to facilitate smooth movement of eyelids during blinking.
Aqueous layer:-
Middle aqueous layer of tear film is secreted by the lacrimal gland and the accessory glands of Krause and Wolfring as depicted in Main bulk of thickness of tear film is constituted by this layer. Aqueous layer comprises 60% of the tear film. Thickness of aqueous layer of precorneal tear film is uniform over the cornea and is about 7 µm. The film covering the cornea is considerably thinner than over the conjunctiva, Recently, it has also been suggested that there are dissolved mucins in the aqueous layer which decrease in concentration towards the lipid layer and form the so-called aqueous-mucinous phase.
Composition: This layer is an aqueous solution of low viscosity, containing ions of inorganic salts, glucose, urea and various biopolymers such as enzymes, proteins and glycoproteins. Lysozyme, lactoferrin, tear specific prealbumin and secretory immunoglobulin-A are the main constituents of protein fraction. Because some bicarbonate ions as well as proteins are present, the tear fluid has some buffering capacity. It has been observed that only the macromolecular solutes of the tears have surface activity. The electrolyte concentration of aqueous layer varies with flow rate. At low flow rates, the fluid is hypertonic whereas at higher flow rates it becomes isotonic.
Surface tension of normal aqueous tears varies between 40 and 42 dyn/cm. All the surface active substances in the aqueous tear that determine its surface tension are macromole cular and believed to be mucous glycoproteins.
Functions: It serves to provide atmospheric oxygen to the epithelium, washes away debris and noxious irritants and contains antibacterial substances like lysozyme and betalysin. Thus the aqueous layer has antibacterial, antiadhesive and lubricant properties.
Mucs Layer:-
Deepest stratum of the precorneal tear film is the mucus coat. Being in a highly hydrated, semisolid state, the mucus layer is not strictly a part of fluid film. It plays a vital role in the stability of the tear film. That is why Holly and Lemps found it reasonable to consider it as the third layer of tear film. They also observed that in healthy eyes the mucus layer is rather thin (only 0.02-0.04 µm), so its morphology usually resembles the microvillous, ridged appearance of superficial epithelial cell walls. However, it has beem suggested that tear mucins are of two types, i.e. aqueous soluble mucins and membrane adherent mucins: and as per recent concepts the mucins dissolved in the aqueous forms the so called aqueous-mucinous phase of tear film.
Mucin layer is mainly secreted by conjunctival goblet cells, crypts of Henle and the glands of Manz. But mucus has also been identified both histochemically and biochemically in the secretions of the main lacrimal gland. Mucus layer is made from the epithelial cell glycocalyx and a layer of tear mucins (glycoprotein). MUC5AC is the main tear mucin which is produced along with the trefail protein TFF1 and 3.
Thickness: Electron micrographs of epithelial sections stained with Mowry’s colloidal iron stain revealed that mucous layer has a thickness ranging from 200-500 Å (0.02 to 0.04 µm).
- Mucin lubricates the ocular and palpebral surfaces, so that minimal energy is lost as friction during and eye movement.