Keratometry is a simple, rapid and non-invasive test. It has some limitations. It measures the curvature of the anterior corneal surface usually across a fixed chord length of 2 to 3 mm which falls within the spherical optic zone of the cornea.
The principle of Keratometry is that the anterior corneal surface behaves as a convex mirror and the size of the image change with the curvature. There are various clinical uses of keratometers such as corneal astigmatism measurement, contact lenses fitting, assessment of refractive error, IOL calculation, etc.
The main criteria for well fitted contact lenses after adaptation is that the keratometer reading donot show a significant change after wearing the lenses.
Corneal anoxia and the retention of metabolites within the tissue lead to corneal edema which causes change in thickness of cornea and the surface shape changing the refractive status of the eye. That is why, measurement of corneal curvature using keratometer during the course of adaptation is an important test to determine whether the adaptation is progressing favorably or not. Marked change in the corneal curvature may indicate an ill fit and this is used as a parameter for refitting the lenses.
Keratometry taken on the front surface of a soft contact lens can reveal the quality of the contact lens surface. If the contact lens becomes coated, mire images will appear indistinct.
In refractive surgery, keratometry is helpful in the pre-evaluation in determining the presence of irregular astigmatism.
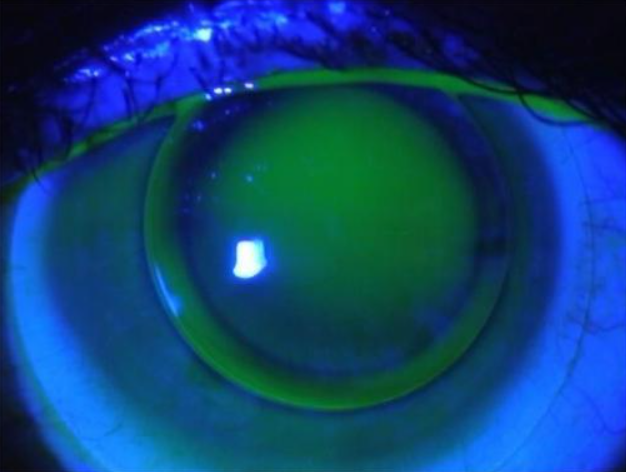
Keratoconus
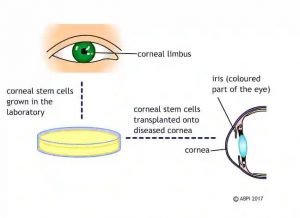
Keratoconus is the abnormal, progressive, bilateral and asymmetrical thinning of the centrum of the cornea. The resultant corneal ectasia, protrusion and disruption of the optics of the cornea occur as a result of pressurized fluid within the eye. The disease usually starts at
childhood and adolescence. In early stages most patients are asymptomatic, except for frequent changes in their eye sight, which represents myopia, regular or irregular and moderate or severe astigmatism. In most cases, the disease is suspected when eyeglasses are unable to correct the vision or when rapid changes in astigmatism develop.
Corneal topographic map reveals regular or irregular increments in corneal power and pachymetry shows gradual decrease in corneal thickness. When the disease is mild, wearing eyeglasses might be enough and sometimes the patients experience better corrected vision in comparison with wearing contact lenses.
Surgery is reserved for the patients who cannot tolerate contact lenses or those who gain no improvement in their vision.
Importance of Keratometry
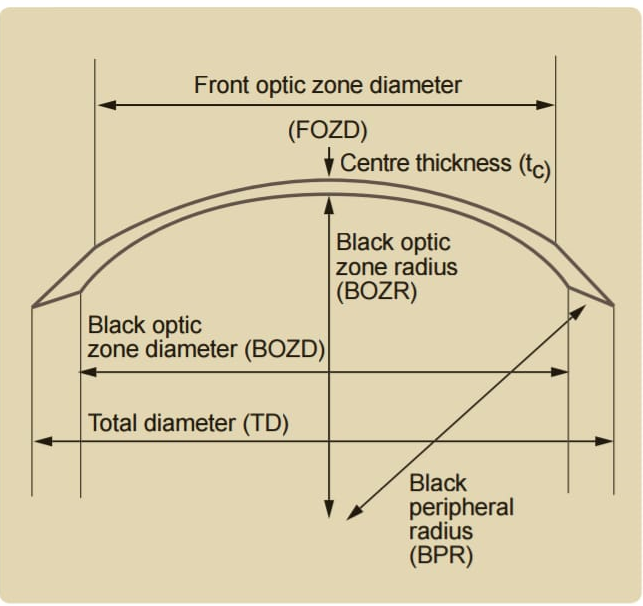
The Keratometry helps in the selection of contact lenses. The variations in the severity of diseases in each patients makes the process of rigid contact lens fit fit lengthy and sometimes inaccurate. The ability to more accurately pick the initial rigid lens base curve based on keratometry reading helps an apprentice fitter to fit the len ses with more confidence.
Although the litreture lacks to provide such level of confidence for the fitter, there are few studies to support the idea. The development of new formulas which could be able to estimate the base curve for each patient due to the keratometry reading not only helps to fit more accurate lenses but also saves the time and cost.
The mathematical correlation between Rigid Gas Permeable Contact Lens base curve and keratometry reading helps the less experienced fitter to pick the initial lenses with more confidence.
Keratometric measurements are critical in fitting contact lenses particularly Rigid Gas Permeable lenses for monitoring corneal pathology and for identifying keratoconus.
If K reading are outside of what is considered a normal range or if there is irregularity in the mires, that instantly clues you into the potential pathology of keratoconus. Now with corneal cross linking, the sooner we identify it, the sooner we can slow down the progression of corneal steepening.