Myopia is the single most significant cause of distance vision impairment, and high myopia (worse than -5.00D) is associated with a number of sight-threatening complications—highlighting the need for strategies and solutions to reduce the risk of onset and slow progression. This article discusses the use of soft contact lenses for myopia control and how to incorporate them into your practice.
Myopia affected approximately one and a half billion people in 2010, and that number is expected to rise to nearly five billion by 2050.1 It is the single most significant cause of distance vision impairment, and high myopia (i.e., worse than -5.00D) is associated with a number of sight-threatening complications such as myopic macular degeneration, retinal detachment, cataract and glaucoma. This significant burden highlights the need for strategies and solutions to reduce the risk of onset and slow the progression in those already affected by myopia.
Strategies for Control
Myopia is a complex trait influenced by a number of environmental and genetic factors, and the mechanisms underlying onset and progression are not fully understood. Although there is a great deal to learn about the mechanisms of myopia and why individuals respond differently to different stimuli and treatments, some behavioural, pharmaceutical and optical strategies already show promise in clinical trials in combating myopia—many of which can be incorporated into current day practice.
Prevention is obviously the most effective strategy to reduce the burden of myopia. Several randomized clinical trials suggest a lifestyle intervention with more time spent outdoors reducing the risk of onset. However, because this involves education and behavioural modification in the years prior to the onset of myopia, comprehensive community-based programs that involve parents, caregivers, teachers, governmental and non-governmental organizations and eye care practitioners (ECPs) must be implemented for this approach to be effective. Despite the crucial role ECPs play in educating parents and communities, their role is limited by the fact that first contact with a practitioner usually comes after the onset of symptoms and signs.
Once a patient is diagnosed with myopia, the ECP becomes the central care provider and is integral to evaluating the risk of further progression. ECPs now have many options for correcting distance vision impairment and slowing its progression. These options include more time spent outdoors, atropine therapy (including low-dose atropine 0.01%), spectacles (progressives, peripheral defocus management and executive bifocals), contact lenses that impose myopic defocus across sections of the retina, and orthokeratology.
Of these various interventions, contact lenses fare well in terms of the risk-benefit ratio compared with other interventions for myopia control. For example, atropine has greater efficacy rates but an increased risk of side effects compared with contact lenses; in addition, myopia rebounds once treatment is stopped. Clinical trials and case studies show specially designed contact lenses slow myopia progression from 25% to 72% compared with spectacles.
Contact lenses used for myopia control can be either bifocal or multifocal soft contact lenses, as well as the rigid contact lens designs used in orthokeratology. Investigators have proposed several mechanisms to explain their myopia control effect, including: (1) contact lenses correct or reduce accommodative lag, which is considered a stimulus for eye elongation; (2) they reduce the peripheral retinal defocus, which is considered to increase the risk of eye elongation by shifting the image closer to the retina; and (3) the lenses impose myopic defocus across areas of the retina, which is considered to inhibit eye growth.
These practice pearls can help you better understand the use of soft contact lenses for myopia control and how to incorporate them into your practice. Currently, no products are on the market specifically for use in myopia control; thus, this discussion is based on clinical trial data on the use of multifocal contact lenses for myopia control.
Where to Begin
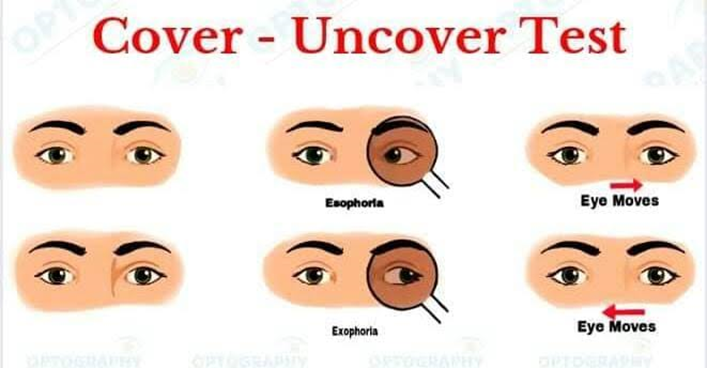
All individuals presenting with myopia should be assessed for risk of progression based on age, ethnicity, family history of myopia and past history of progression. The ocular examination should include a cycloplegic assessment of the refractive error. A non-cycloplegic refraction often results in a more myopic refraction, and the difference is greatest in younger children and those with low myopic, emmetropic and hyperopic refractive errors.27 Because of this, ECPs should note that a patient without myopia could be classified incorrectly as having myopia; likewise, the magnitude of myopia could be found to be higher than it actually is in a patient with myopia.
Contact lenses versus spectacles in myopia
There are many benefits for fitting myopic – notably highly myopic – individuals into contact lenses versus maintaining spectacle wear. The overall field of view is greater (100˚ versus 80˚ with spectacles), fewer optical aberrations are present as the patient views through the optical centre of the lens at all times, the eyes do not appear as minified to the viewer and contact lenses increase the magnification of the retinal image, and the induced prismatic effects with oblique gaze are eliminated. The only possible compromise would be the pre-presbyopia high myope who loses the Base In effect achieved with spectacles during near work, requiring more convergence and accommodation and possibly necessitating a near correction earlier than with spectacles.
Fitting Age
Studies show children as young as eight can successfully manage lens insertion, removal and care. Other clinical studies found children achieved the required duration of lens wear (including full-time lens wear), and the reported duration of lens wear was comparable with that seen in adult contact lens wearers. Evidence shows no increased risk of complications associated with lens wear in children compared with adults. While it is common practice to teach both the child and the parent, the ECP should ensure the child can independently manage all aspects of lens wear before prescribing them.
In addition to correcting and controlling progression of myopia, studies indicate children and teenagers wearing contact lenses had improved quality of life with respect to appearance and satisfaction with correction. However, not all children can successfully wear contact lenses. Conditions such as allergic conjunctivitis have an onset in childhood and, in such instances, contact lens wear may aggravate or increase the risk of flare-up. Clinicians should ask about any previous history of allergic or vernal conjunctivitis, and examinations should include an eversion of the tarsal conjunctiva.
Rigid gas permeable (GP) lens: applications, design and fitting
Lens Materials
The use of silicone-acrylate lens materials has been replaced by fluoro-silicone/acrylate(F-S/A) materials which provide greater oxygen permeability, wettability and stability than their predecessors.
Applications
The most important application of GP lenses is for patients desiring – or benefitting from – good quality of vision. Notably moderate- to-high astigmatic, irregular cornea, and presbyopic individuals benefit from both the ability to mould the front surface of the cornea and the optical quality of GP lenses. Special design GPs are not within the scope, but it has recently been found that when highly astigmatic subjects wore both soft toric and GP lenses, almost 75% preferred the vision of the GPs and the majority elected to stay in them This is consistent with studies comparing spherical GP to spherical soft lenses.GP lenses have also demonstrated an ability to reduce spherical aberration when worn and, in fact, when subjects were corrected with multiple modalities it has been found that correction with GP lenses resulted in significantly better optical quality than soft lenses or spectacle lenses.
Design and Fitting
The smaller size of GP lenses, resulting in greater movement on the eye and more initial lid sensation and lens awareness, in addition to their custom lens design, have deterred practitioners from fitting GP lenses to many patients who would benefit from this modality. However, presenting GPs in a positive but realistic manner, use of a topical anaesthetic immediately prior to initial lens application, and lens design improvements can all result in a positive initial experience for the myopic patient. Lens designs in common use today have larger overall diameters (often 9.5 – 10.5mm) resulting in less movement on the eye, ultrathin profiles – reducing lens mass and optimizing centration, and aspheric or pseudo-aspheric peripheries to better align the lens to the cornea. The use of a plus lenticular with high (often ≥ 5D) minus lenses reduces the edge thickness to optimize comfort while allowing a better view of the peripheral fluorescein pattern. In addition, new corneal-scleral designs (13.5 -16mm) are now being advocated for first-time myopic contact lens wearers. All of these factors should optimize initial comfort.
Conclusion
Contact lens correction of myopic has never been more exciting with new generation Si-Hy lens materials, large diameter GP lenses in hyper transmissible materials, and third generation hybrid lenses. With improvements in special design lenses for high astigmatic, presbyopic, and irregular cornea patients, the future looks even better.