Introduction
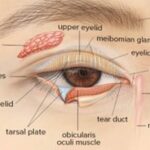
Vernal keratoconjunctivitis (VKC) is a recurrent, bilateral allergic inflammation of the conjunctiva. The episodes are often periodic and have seasonal recurrences. Seasonal exacerbations characterize the condition in the initial stages with a peak incidence during spring and summer. Over time, the condition tends to become perennial. VKC is a subtype of allergic conjunctivitis. Vernal keratoconjunctivitis (VKC) is a type of allergic conjunctivitis. Additional types include perennial and seasonal rhino conjunctivitis, atopic keratoconjunctivitis, and giant papillary conjunctivitis. VKC is classified
based on the area of ocular involvement into palpebral, limbal, and mixed
forms.
Palpebral VKC
This involves the upper tarsal conjunctiva. There is a close association between the inflamed conjunctiva and the corneal epithelium, often leading to significant corneal disease.
Limbal VKC
This typically affects bulbar conjunctiva in the palpebral area and typically affects the Black and Asian populations.
Mixed VKC
This has features of both the palpebral and limbal forms.
Etiopathogenesis
Vernal keratoconjunctivitis (VKC) is found in individuals with predisposed
atopic background. It has long been considered an atopic disorder, mainly
type-I IgE-mediated hypersensitivity reaction to pollen allergens. However,
now it is believed that pathogenesis of VKC is characterized by Th2
lymphocyte alteration and that the exaggerated IgE response to common
allergens is a secondary event.
Predisposing factors
1. Age and sex. 4-20 years; more common in boys than girls.
2. Season. More common in summer; hence the name spring catarrh seems to be a misnomer. Recently, it is being labelled as ‘Warm weather conjunctivitis. Seasonal exacerbation, is common, but patients may have symptoms year-round.
3. Climate. More prevalent in tropics, less in temperate zones and almost non-existent in cold climate.
4. Other atopic manifestations, such as eczema or asthma, are associated inn 40-75% patients with le VKC.
5. Family history of atopy is found in 40-60% of patients. Pathology
1. Conjunctival epithelium in papillary region contains large number of mast cells, eosinophils and undergoes hyperplasia and sends downward projections into the subepithelial tissue.
2. Adenoid layer shows marked cellular infiltration by mast cells eosinophils, plasma cells, lymphocytes and histiocytes.
3. Fibrous layer shows proliferation which later on undergoes hyaline changes.
4. Conjunctival vessels also show proliferation, increased permeability and vasodilation. All these pathological changes lead to formation of multiple papillae in the upper tarsal conjunctiva.
Clinical features
Symptoms:
Spring catarrh is characterized by:
• Marked burning and itching sensation which is usually intolerable and accentuated when patient comes in a warm humid atmosphere. Itching is more marked with palpebral form of disease.
• Other associated symptoms include: mild photophobia, lacrimation, stringy (ropy) discharge and heaviness of lids.
Evaluation
The diagnosis of vernal keratoconjunctivitis is based on clinical examination. The typical history and clinical signs lead to a straightforward diagnosis in most cases. Different staining techniques and associated scoring systems have been described to grade the severity of VKC. The fluorescein stain, lissamine green stain, and confocal microscopy are a few evaluation techniques that help score
the severity and grade of involvement. Studies have proven that Oxford scores and Van Bijsterveld scores for evaluating epithelial damage are useful in patients with VKC. Further, the VKC-Collaborative Longitudinal Evaluation of Keratoconus Study (VKC-CLEK) was found to be useful in assessing both limbal and tarsal epithelial damage in VKC patients.
Differential diagnosis
The close differentials of vernal keratoconjunctivitis include all types of allergic conjunctivitis, including seasonal allergic conjunctivitis, perennial allergic conjunctivitis, atopic keratoconjunctivitis, giant papillary conjunctivitis. Most of these are IgE mediated responses except giant papillary conjunctivitis. None have gender predilection, except AKC and VKC, which are more prevalent among males. History
and physical examination often help in distinguishing between these clinical entities.
Management
A. Topical anti-inflammatory therapy
Topical anti-inflammatory therapy with combined steroids, mast cell stabilizers, antihistamines, and NSAIDs forms the mainstay of treatment of VKC.
1. Topical steroids: These are effective in all forms of spring catarrh. However, their use should be minimized, as they frequently cause steroid induced glaucoma. Therefore, monitoring of intraocular
pressure is very important during steroid therapy. Frequent instillation (2 hourly) to start with (7 days) should be followed by maintenance therapy for 4 times a day for 2 weeks.
Commonly used steroid solutions are of fluorometholone, medrysone, betamethasone or dexamethasone. Medrysone and fluorometholone are safest of all these.
2. Mast cell stabilizers such as sodium cromoglycate (2%) drops 5 times a day are quite effective in controlling VKC, especially atopic cases.
3. Dual action antihistamines and mast cell stabilizers such as azelastine, olopatadine and ketotifen are very effective for control and prevention of exacerbations.
4. NSAIDs eye drops such as ketorolac and diclofenac give added benefits.
5. Topical cyclosporine (0.5 to 1%), the immune-modulator , is indicated when steroids are ineffective,Inadequate, or poorly tolerated, or when given as a steroid-sparing agent in patients with severe disease.
6.Tacrolimus (0.03% ointment) is another immune- modulator, which can be useful in refractory cases.
B.Topical lubricating and mucolytics
1.Artificial tears, such as carboxymethyl cellulose, provide soothing effect.
2.Acetyl cysteine (0.5%) used topically has mucolytic properties and is useful in the treatment of early plaque formation.
C. Systemic therapy
1.Oral antihistaminics may provide some relief from itching in severe cases.
2.Oral steroids for a short duration have been recommended for advanced, very severe, non- responsive cases.
D. Treatment of large papillae Very large (giant) papillae can be tackled either by:
Supratarsal injection of long acting steroid, or
Cryo application, or
Surgical excision is recommended for extraordi- narily large papillae.
E.Supportive measures include:
• Dark goggles to prevent photophobia.
• Cold compresses and ice packs have soothing effects.
• Maintenance of air conditioned atmosphere.
F. Desensitization
Desensitization has also been tried without much rewarding results.
G. Treatment of vernal keratopathy
• Punctate epithelial keratitis requires no extra treatment except that
instillation of steroids should be increased.
• A large vernal plaque requires surgical excision by superficial keratectomy.
• Severe shield ulcer resistant to medical therapy may need surgical treatment in the form of debridement, superficial keratectomy excimer laser therapeutic keratectomy as well as amniotic membrane transplantation to enhance re-epithelialization. Complications
The ocular complications reported among vernal keratoconjunctivitis patients include steroid-induced cataract, steroid-induced glaucoma, irregular astigmatism, keratoconus, acute hydrops, shield ulcer, central corneal scars, and limbal tissue hyperplasia.