Funduscopic examination is a routine part of every doctor’s examination of the eye, not just the ophthalmologist’s. It consists exclusively of inspection. One looks through the ophthalmoscope which is simply a light with various optical modifications, including lenses. The ophthalmoscope illuminates the retina through the normal iris defect that is the pupil. Light rays forming the image of the retina re-emerge through the pupil. The viewing aperture (window) of the ophthalmoscope contains a lens that modifies light rays to assist the user. In the procedure, one looks at structures lying in the innermost aspect of the globe, collectively known as the eyegrounds: retina, retinal blood vessels, optic nerve head (disk), and to a limited degree, subjacent choroid. The pupil is frequently dilated pharmacologically to render retinal inspection easier, and for examination of the macula. One paralyzes the pupilloconstrictor muscle of the iris with nonabsorbable, short-acting topical parasympatholytic drugs, resulting in a larger pupillary aperture. In comparison to the ophthalmologist, the internist, neurologist, or pediatrician concentrates particularly on funduscopic manifestations of systemic disease and less on local ocular disease. Synonyms for funduscopic examination include funduscopy, ophthalmoscopy, and direct ophthalmoscopy. Only ophthalmologists perform retinoscopy and indirect ophthalmoscopy, which require other equipment and provide different information.
Clinical Significance:
Funduscopy provides the only means for direct inspection of arteries, veins, or central nervous system in the intact, living patient. Any list of conditions in which it changes patient management and outcome would be woefully incomplete. A few selections are cited.
The finding of papilledema, that is, a swollen optic nerve-head usually reflecting elevated intracranial pressure, is a medical emergency. Treatment of its cause will prevent irreversible neuronal damage and somatic death. The absence of papilledema does not mean that all is well, since its development does not occur immediately after intracranial pressure rises. However, visible retinal venous pulsations exclude increased intracranial pressure, a vital datum in assessing any patient with headaches, an evolving neurologic status, or head trauma. Loss and reappearance of pulsation rapidly reflect intracranial pressure changes. Importantly, absent pulsations do not necessarily mean elevated intracranial pressure.
Retinal hemorrhages occur in diverse conditions including endocarditis, pernicious anemia, diabetes mellitus, leukemia, subarachnoid hemorrhage, and disseminated intra-vascular coagulation (DIG). They always deserve note in diagnosis and management; their appearance may lead to an initial diagnosis, or to assessment of progression. In severe hypertension, finding a retinal hemorrhage redefines the entity as accelerated hypertension; no given blood-pressure reading can do this. The grim prognosis of this entity, if uncontrolled, constitutes an emergency in which blood pressure control is needed not over weeks but in a day. Often this means treatment in the intensive care unit. The prevention of early death, preservation of renal function, and feasibility of subsequent outpatient maintenance reward the examiner’s prowess.
The chorioretinal lesions of certain infections are virtually diagnostic in and of themselves. Candidal exudates mean endophthalmitis in the patient with suspected systemic candidosis. Cytomegalovirus in the patient with AIDS has a highly characteristic appearance that consists of mixed hemorrhages and yellow granular exudates, both frequently centered on vessels. A vivid if offensive aide-memoire for this appearance is “crumbled cheese and ketchup”. Toxoplasmosis and histoplasmosis of the eye also have distinct although not pathognomonic looks on physical examination by funduscopy. Miliary tuberculosis may be confirmed by spotting choroidal tubercles.
The (apparent) complete obliteration of venous blood columns where they cross arteries, when it occurs more than two disk diameters away from the disk, is called complete AV (arterio-venous) crossing change.
Proliferative diabetic retinopathy is a leading cause of blindness, but can be contained with laser photocoagulation. Ophthalmoscopic recognition of pre-proliferative lesions, or of frank neovascularization, will lead to measures to prevent its occurrence, and its typical sequelae of retinal and vitreous hemorrhage, and permanent blindness.
Diabetic nephropathy rarely occurs without diabetic retinopathy, so a normal retina in a nephrotic diabetic will stimulate a search for nondiabetic causes of renal disease, thus refining selective and efficient use of diagnostic resources.
In cerebrovascular disease, an ophthalmoscopic finding provides data essential for management. If the examiner sees fragments of atheroma impacted in retinal arterioles, she knows that they did not originate in situ, as this caliber of vessel does not experience atherogenesis. Therefore they have embolized from an ulcerated plaque in a more proximal locale, such as the aortic arch or a carotid artery. Such fragments are yellow and refractile, and typically occlude an arteriolar branch; they are called Hollenhontplaques. The hazard of further embolization to the brain will strengthen the case for carotid arterial surgery. Most cerebrovascular tests measure brain texture, blood flow, or pressure; all of these may remain normal if an ulcerated plaque occurs without critical arterial stenosis; carotid arteriography is an exception, but its danger, discomfort, and expense relegate it to highly selected cases, so that the need to use funduscopy for screening is underscored.
Tortuous “sausage-link-like” retinal veins in the patient with macroglobulinemia imply marked hyperviscosity and will heighten antithrombotic efforts.
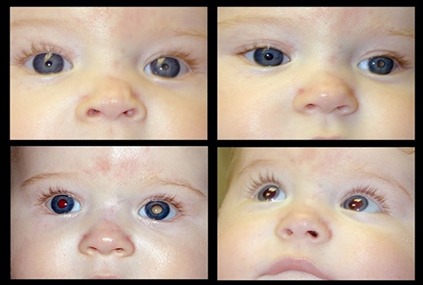
The discovery of retinoblastoma, a childhood malignancy that is sometimes familial, will lead to lifesaving therapy and prevention for the patient and perhaps for other family members as well. Surveillance of the remaining eye post enucleation may uncover a second primary, which afflicts many victims; if found early enough, conservative therapy may preserve vision as well as life.