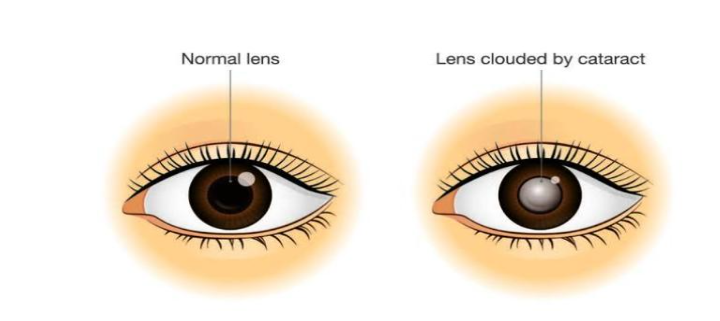
Congenital cataracts are a lens opacity that is present at birth. Congenital cataracts
occur in a broad range of severity. Some lens opacities do not progress and are visually
insignificant, others can produce profound visual impairment. Congenital cataracts are
considered to be a significant cause of childhood blindness. This condition is considered
'treatable' with early intervention and compared to other types of childhood visual loss
problems, however, in parts of the world where treatment options are not available such
as some low-income countries, the condition may go untreated and the person may lose
their vision. Early in life treatment is important, especially during development, in order
that the person's eyes and visual system develops normally.
Types Of Congenital Cataract –
A. Nuclear Cataracts-
Cataracts affecting the center of the lens, called nuclear cataracts. A nuclear
cataract may at first cause objects far away to be blurry but objects up close to
look clear.
B. Cerulean Cataracts-
Cerulean cataracts, also known as blue dot cataracts, are developmental
cataracts characterized by blue and white opacifications scattered in the nucleus
and cortex of the lens. Patients with cerulean cataracts are usually asymptomatic
until 18-24 months of age and often do not need them removed before
adulthood.
C. Posterior polar Cataracts-
Posterior polar cataract (PPC) is a unique form of congenital cataract, which
results in defective distance and near vision and affects the patient's daily
activities.
Signs and symptoms-
Congenital cataracts occur in a variety of morphologic configurations, including lamellar,
polar, sutural, coronary, cerulean, nuclear, capsular, complete, membranous. Some
signs that a child may have a cataract can the child being unable to follow faces or
objects, inward or outward deviation of one or both eyes, shaking of one or both eyes,
and/or the presence of white reflex in one or both eyes.
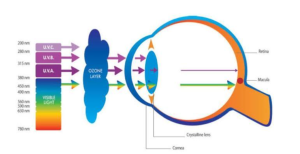
Cause-
In general, approximately one-third of congenital cataracts are a component of a more
extensive syndrome or disease (e.g., cataract resulting from congenital rubella
syndrome), one-third occur as an isolated inherited trait, and one-third result from
undetermined causes. Metabolic diseases tend to be more commonly associated with
bilateral cataracts.
Genetic & Metabolic-
-Down syndrome
-Hallermann-Streiff syndrome
-Lowe syndrome
-Galactosemia
-Cockayne syndrome
-Marfan syndrome
-Hypoglycemia
-Alport syndrome
-Myotonic dystrophy
-Fabry disease
-Hypoparathyroidism
-Conradi syndrome
Infections-
-Toxoplasmosis
-Rubella
-Cytomegalovirus
-Herpes Simplex
Anomalies-
-Aniridia
-Anterior segment dysgenesis
-Persistent fetal vasculature (PFV)
-Posterior lenticonus
Toxic-
-Corticosteroids
-Radiation
Diagnosis-
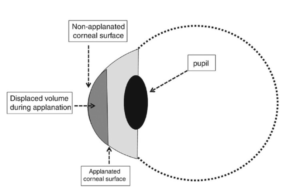
-The red reflex test is best performed in a darkened room and involves shining a bright
direct ophthalmoscope into both eyes simultaneously from a distance of 1– 2 ft. This
test can be used for routine ocular screening by nurses, pediatricians, family
practitioners, and optometrists.
-Retinoscopy through the child's undilated pupil is helpful for assessing the potential
visual significance of an axial lens opacity in a pre-verbal child. Any central opacity or
surrounding cortical distortion greater than 3 mm can be assumed to be visually
significant.
Treatment-
Surgery:
In general, the younger the child, the greater the urgency in removing the cataract,
because of the risk of amblyopia during development. For optimal visual development in
newborns and young infants, a visually significant unilateral congenital cataract should
be detected and removed before age 6 weeks, and visually significant bilateral
congenital cataracts should be removed before age 10 weeks.Surgical options if the
cataracts are bilateral and the vision is compromised include removing the affected lens
of the eye and correcting the vision as early as possible so that the infants eyes can
develop normally with visual stimuli.
Some congenital cataracts are too small to affect vision, therefore no surgery or
treatment will be done. If they are superficial and small, an ophthalmologist will continue
to monitor them throughout a patient's life. Commonly, a patient with small congenital
cataracts that do not affect vision will eventually be affected later in life; generally this
will take decades to occur.
Prognosis-
The prognosis for a congenital cataract varies based on several factors. These factors
include clouding of the lens present at birth, time of detection, and effectiveness of
treatment. When detected early, a congenital cataract has the most favorable outcome.
Most cases of congenital cataracts require surgery to remove the cataract, but
advancements in pediatric ophthalmology and surgical techniques have significantly
improved success rates. Prompt surgical intervention can help restore vision. Early
intervention can also prevent long-term conditions such as amblyopia, also known as
lazy eye. The prognosis may be influenced by associated conditions or complications.
Follow-up care is essential to monitor visual development and address any potential
challenges that may arise. With timely and appropriate management, many individuals
with congenital cataracts can achieve good visual outcomes and lead fulfilling lives.
Epidemiology-
– Congenital cataracts are responsible for nearly 10% of all vision loss in children
worldwide.
– Congenital cataracts are one of the most common treatable causes of visual
impairment and blindness during infancy, with an estimated prevalence of 1 to 6 cases
per 10,000 live births.