Ocular rigidity refers to the stiffness or
resistance of the eyeball to deformation. It’s a measure
of the eye’s ability to maintain its shape when subjected
to external forces, such as changes in intraocular
pressure. In simpler terms, it’s how “stiff” or “flexible”
the eye is. This rigidity is mainly determined by the
structural integrity of the eye’s outer layers, particularly
the sclera (the white outer layer) and the cornea (the
transparent front part of the eye). Various factors can
influence ocular rigidity, including age, genetics, and
certain eye conditions.Changes in ocular rigidity can have
clinical implications, particularly in conditions like
glaucoma, where alterations in intraocular pressure can
affect the health of the optic nerve. Monitoring ocular
rigidity can provide insights into the biomechanics of the
eye and help in understanding and managing eye
diseases.
1. Components of Ocular Rigidity:
A. Sclera: The outermost layer of the eye, composed of
tough, fibrous tissue, provides structural support and
strength.
B. Cornea: The transparent front part of the eye,
responsible for focusing light onto the retina and
contributing to the eye’s overall shape and rigidity.
2. Factors Influencing Ocular Rigidity:
A. Age: Changes in the composition and organization of
collagen fibers within the sclera can occur with aging,
potentially affecting ocular rigidity.
B. Genetics: Genetic factors can influence the inherent
stiffness and structural integrity of the eye.
C. Diseases: Conditions such as keratoconus,
characterized by corneal thinning and bulging, can
impact ocular rigidity.
3. Clinical Significance:
A. Glaucoma: In glaucoma, an imbalance in intraocular
fluid dynamics can lead to increased intraocular pressure.
Changes in ocular rigidity can affect how the eye
responds to fluctuations in pressure, potentially
contributing to optic nerve damage and vision loss.
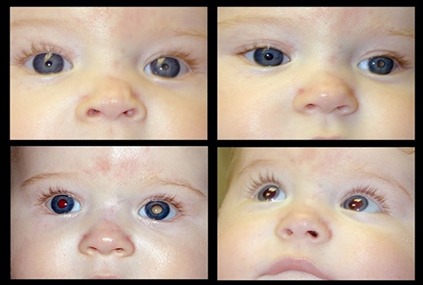
B. Monitoring Eye Health: Understanding ocular rigidity
is crucial for diagnosing and managing various eye
conditions. Techniques such as ocular biomechanical
measurements and imaging technologies help assess
ocular rigidity, providing valuable information for
treatment planning and disease monitoring.
4. Advancements in Research:
A. Ongoing research aims to further elucidate the
biomechanics of ocular rigidity and its role in eye health
and disease.
B. By understanding the factors that influence ocular
rigidity, researchers hope to develop new strategies for
preserving vision and improving outcomes for patients
with ocular conditions.
5. Measurement Techniques :
A. Ocular response analyzer (ORA): Measures corneal
biomechanical properties, providing insights into corneal
hysteresis and corneal resistance factor.
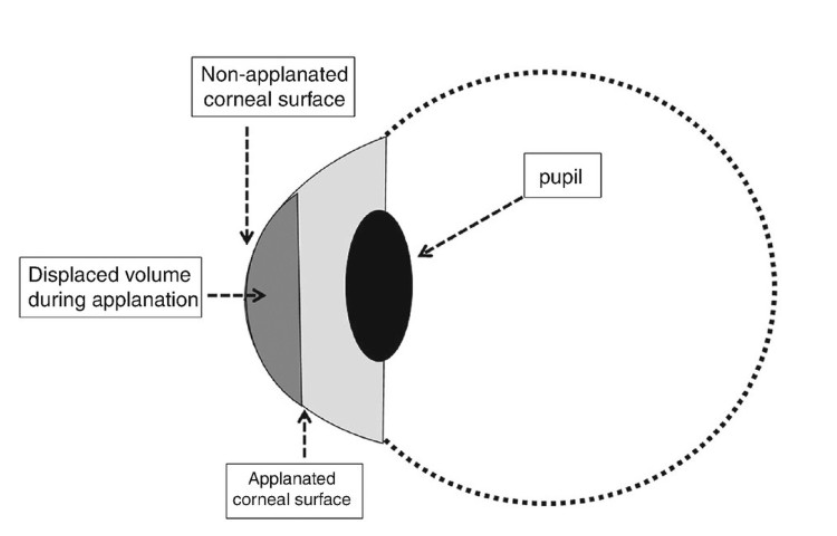
B. Dynamic contour tonometry (DCT): Utilizes a dynamic
sensor to measure intraocular pressure and estimate
ocular rigidity by analyzing the response of the eye to
indentation.
C. Ocular coherence elastography (OCE): Uses imaging
technology to assess the mechanical properties of ocular
tissues non-invasively.
6. Implications for Surgical Procedures:
A. In refractive surgery, such as LASIK (laser-assisted in
situ keratomileusis), understanding ocular rigidity is
crucial for predicting postoperative corneal shape
changes and refractive outcomes.
B. Similarly, in intraocular surgery, such as cataract
extraction or implantation of intraocular lenses,
considerations of ocular rigidity may influence surgical
techniques and implant selection to optimize visual
outcomes.
Conclusion:
Ocular rigidity, reflecting the eye’s resistance to
deformation, is a fundamental aspect of ocular
biomechanics with significant clinical implications.
Influenced by factors such as age, genetics, and ocular
diseases, understanding ocular rigidity aids in the
diagnosis, management, and surgical treatment of
various eye conditions, particularly glaucoma. Advanced
measurement techniques and ongoing research efforts
continue to deepen our understanding of ocular rigidity,
paving the way for improved diagnostic accuracy,
treatment outcomes, and preservation of vision. By
integrating knowledge of ocular rigidity into clinical
practice, eye care professionals can enhance patient care
and contribute to the advancement of ophthalmic
science and technology.