Uveitis is inflammation of the uveal tract of the eye, which includes the iris, ciliary body,
and choroid. It can be unilateral or bilateral, if not treated it can be lead to serious
complications.
Types of uveitis
1. Anterior Uveitis :- It involves iris and ciliary body so it is name as iritis and iridocyclitis
Features:- It can be happen sudden onset and it can be usually unilateral but
sometimes it can be bilateral.
Symptoms:
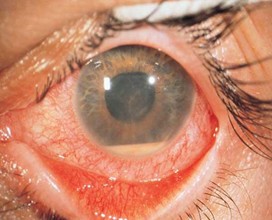
Severe and moderate Eye pain , redness which can seen around the eye, light
sensitivity which is called photophobia, tearing , Blurred or dimnished vision.
Signs:
Cells and flare in the anterior chamber, Keratic precipitates which deposits on the
corneal endothelium ,posterior synechiae ,small, irregular pupil due to inflammation.
2. Intermediate Uveitis :- It involves pars plana region of the ciliary body and vitreous
Features: it can be unilateral but seen bilateral in many cases, it can be seen in younger adults.
Symptoms:
Floaters – Floaters are small, shadowy shapes like dots, threads, or cobwebs that appear in the visual field, often more noticeable against bright backgrounds Mild blurred vision seen It is normally painless.
Signs:
Vitreous cells and haze
Snowballs (inflammatory clumps in vitreous)
Snowbanking (white exudates on pars plana)
Associated Conditions: Multiple sclerosis (MS),sarcoidosis
3. Posterior Uveitis :-
Involves: Posterior uveitis affect posterior part of the eye which are retina and choroid.
Features:
It can be unilateral or bilateral , vision-threatening if not managed properly
Symptoms:
Floaters can be seen ,blurred or decreased vision, scotomas dark spots seen in visual field metamorphopsia (distorted vision)
Signs:
Choroidal or retinal lesions, retinitis ,vasculitis, swollen of the optic disc.
Causes:
Infections: Toxoplasmosis (most common), CMV, TB, syphilisutoimmune diseases
4. Panuveitis:- It involves all layers of the eyeanterior chamber, vitreous, and
retina/choroid
Features:
Severe inflammation of the eye , it can be seen very often bilateral, sometimes it can be
difficult to treat.
Symptoms:
Combination of symptoms from other types (redness, pain, floaters, vision loss)
Signs:
Extensive inflammation in all ocular segments
Associated With:
Behçet’s disease – Behçet’s disease is a chronic, multisystem inflammatory disorder
characterized by recurrent oral and genital ulcers, uveitis, and skin lesions. It is an
autoimmune vasculitis affecting both arteries and veins of all sizes.
Sympathetic ophthalmia – Sympathetic ophthalmia is a rare, bilateral granulomatous
panuveitis that occurs after a penetrating injury or surgery to one eye, leading to
inflammation in both the injured and uninjured eye.
Vogt-Koyanagi-Harada (VKH) syndrome – VKH syndrome is a rare, multisystem
autoimmune disease targeting melanocyte-containing tissues, leading to bilateral
granulomatous panuveitis along with neurological, auditory, and integumentary
symptoms.
Diagnosis of uveitis –
1. Clinical History:
Onset and duration :- It is observed by when and it is mild or not mild
Laterality – Unilateral or bilateral can be observed.
Systemic symptoms – it can be seen joint pain, rashes, respiratory issues
Past infections or autoimmune diseases
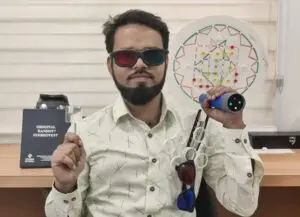
2. Ocular Examination:-
Visual acuity can be recorded by different types of chart.
Slit-lamp exam to detect: Cells and flare in anterior chamber, keratic precipitates,
anterior or Posterior synechiae
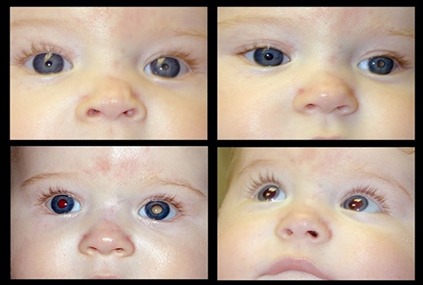
Fundus exam for posterior segment involvement such as involvement of vitreous (
vitritis), choroid involvement ( choroiditis) ,and retinal involvement.
3. Ancillary Tests (if needed):
Intraocular pressure measurement by Schiotz tonometer or applanation tonometer
Ocular imaging: Ocular Coherence Tonography can be used to check macular oedema
Fundus fluorescein angiography
Ultrasound B-scan
4. Systemic Workup:
Blood tests: CBC, ESR, CRP, HLA-B27, ANA, ACE, VDRL, TPHA
Chest X-ray or CT scan: for TB or sarcoidosis
Mantoux test, Quantiferon-TB, Serologies for toxoplasmosis, syphilis, HIV
Autoimmune panel (if suspected)
5. Special Tests:
Aqueous or vitreous tap for PCR or culture in infectious cases
Treatment of Uveitis
1. Control Inflammation:
Corticosteroids:
Topical corticosteroids ( prednisolone acetate) are used for anterior uveitis to reduce
inflammation in the front part of the eye.Systemic corticosteroids ( oral prednisone) are
used for intermediate, posterior uveitis, or panuveitis when the inflammation affects
deeper parts of the eye.Periocular or intravitreal corticosteroids may be used for more
severe cases that don’t respond to topical therapy.
Cycloplegics/Myadriatics:
Atropine or cyclopentolate is used to dilate the pupil and relieve pain by relaxing the
ciliary muscle and preventing synechiae (adhesions between the iris and lens). They
also help in managing photophobia.
2. Treat Underlying Cause:
Infectious Uveitis: If the uveitis is caused by an infection ( tuberculosis, herpes, syphilis,
toxoplasmosis), antibiotics, antivirals, or antifungals are used based on the specific
pathogen.
Autoimmune or Chronic Uveitis:-Immunosuppressive drugs such as methotrexate,
azathioprine, or cyclophosphamide are used for cases of autoimmune-related uveitis or
chronic, recurring inflammation.Biologic agents like infliximab or adalimumab may be
used for refractory or severe cases that do not respond to traditional treatments.
3. Prevent Complications:
Glaucoma Management:
Elevated intraocular pressure (IOP) can occur due to steroid use or inflammation.
Medications like beta-blockers, prostaglandin analogs, or carbonic anhydrase inhibitors
are used to manage glaucoma.
Cataract Formation:
Long-term corticosteroid use can lead to cataract development. Surgical intervention
(cataract surgery) may be needed if vision is significantly impaired.
Macular Edema:
For macular edema (swelling of the macula), which can lead to vision loss, anti-VEGF
injections (e.g., Ranibizumab) or intravitreal corticosteroids may be used.
Regular monitoring and follow-up Care:-
Regular follow-up visits are essential to monitor the effectiveness of treatment,
inflammation levels, and potential side effects. Monitoring for complications such as
glaucoma, cataracts, and macular edema is important to adjust treatment accordingly.
This treatment plan aims to control inflammation, treat the underlying cause, and
prevent long-term complications. Regular follow-ups ensure that the condition is well-
managed and complications are avoided.