Treatment of modern Cataract Surgery
Cataracts, a common condition where the lens of the eye becomes cloudy, affecting vision, have been a significant challenge throughout history. However, modern cataract surgery has revolutionized the treatment of this condition, making it one of the safest and most
effective procedures in medicine today.
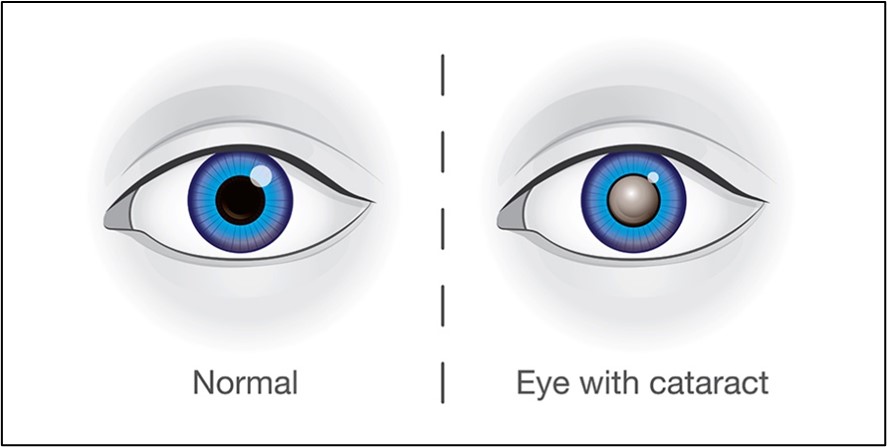
Understanding Cataracts Cataracts primarily affect older adults, although they can occur at any age due to various factors such as genetics, trauma, or certain medications. Symptoms include blurry vision, difficulty seeing at night, sensitivity to light, and seeing halos around lights. When these symptoms start to interfere with daily activities, surgery becomes necessary.
Evolution of Cataract Surgery
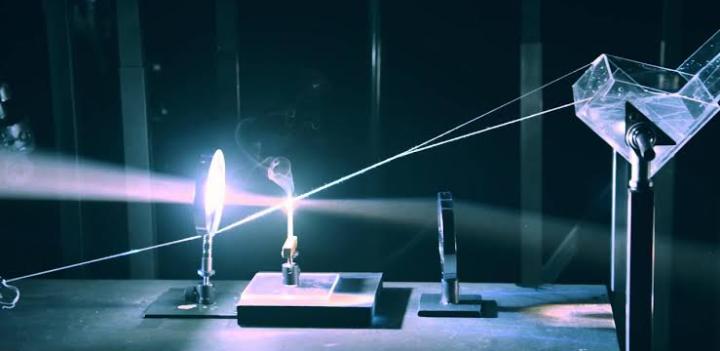
The evolution of cataract surgery is a fascinating journey. Early techniques involved making a 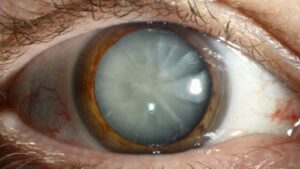 large incision to remove the cloudy lens, followed by wearing thick glasses or contact lenses to compensate for the loss of the natural lens. These methods were far from perfect and carried significant risks. The turning point came in the mid-20th century with the development of intraocular lenses (IOLs) and the advent of phacoemulsification. This
large incision to remove the cloudy lens, followed by wearing thick glasses or contact lenses to compensate for the loss of the natural lens. These methods were far from perfect and carried significant risks. The turning point came in the mid-20th century with the development of intraocular lenses (IOLs) and the advent of phacoemulsification. This
technique, pioneered by Dr. Charles Kelman in the 1960s, uses ultrasonic energy to emulsify the cloudy lens, which is then aspirated out of the eye. This method allows for a much smaller incision, reducing healing time and the risk of complications.
Modern Cataract Surgery Techniques
Today’s cataract surgery is a highly refined procedure, characterized by several key
advancements:
1.Minimally Invasive Procedures:
Phacoemulsification remains the gold standard. The surgeon makes a tiny incision, often less than 2.8mm, uses an ultrasonic probe to break up the cataract, and suctions out the fragments. Femtosecond Laser-Assisted Cataract Surgery (FLACS)* is a more recent innovation. A femtosecond laser creates precise incisions and breaks up the cataract, which can lead to even more accurate results and potentially faster recovery.
2.Intraocular Lenses (IOLs)
Modern IOLs have transformed postoperative vision outcomes. Traditional monofocal 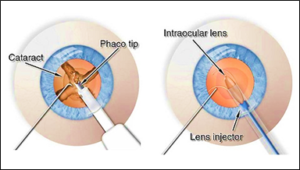 lenses provide clear vision at one distance, typically set for distance vision. Multifocal IOLs and accommodative IOLs offer clear vision at multiple distances, reducing dependence on glasses. Toric IOLs are designed to correct astigmatism, providing sharper vision for those with this
lenses provide clear vision at one distance, typically set for distance vision. Multifocal IOLs and accommodative IOLs offer clear vision at multiple distances, reducing dependence on glasses. Toric IOLs are designed to correct astigmatism, providing sharper vision for those with this
refractive error.
3.Advanced Imaging and Diagnostics:
Preoperative imaging technologies, like optical coherence tomography (OCT) and intraoperative aberrometers, allow for precise measurements and customization of the surgical approach. This ensures that the IOL is perfectly suited to the patient’s eye,
optimizing visual outcomes.
4.Enhanced Surgical Tools:
Innovations in surgical tools, such as microincision instruments and advanced viscoelastic substances, enhance the surgeon's ability to perform the procedure with minimal trauma to the eye.
The Surgical Procedure
A typical modern cataract surgery involves several well-orchestrated steps:
1.Preoperative Preparation:
The patient undergoes a comprehensive eye examination to determine the extent of the cataract and measure the eye's dimensions. This includes assessing the corneal curvature and the length of the eye to select the appropriate IOL. Local anesthesia, usually in the
form of eye drops, is administered to numb the eye. Sedation may also be provided to help the patient relax.
2.Surgical Steps:
Incision: A small incision is made at the edge of the cornea.
Capsulorhexis: A circular opening is created in the lens capsule to access the cataract.
Phacoemulsification or FLACS: The cataract is broken up and removed.
IOL Insertion: The selected IOL is inserted into the lens capsule. Closing the Incision: The small incision is self-sealing, often requiring no stitches.
3.Postoperative Care:
Patients are typically prescribed antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation. Follow-up visits are scheduled to monitor healing and ensure optimal vision restoration.
Benefits and Risks
Modern cataract surgery boasts a high success rate, with over 95% of patients experiencing
significant improvement in vision. The benefits include:
-Rapid recovery time.
– Minimal discomfort.
– Reduced dependency on glasses.
– High precision and customization to individual needs.
However, like any surgical procedure, cataract surgery carries some risks, though they are rare. These can include infection, bleeding, retinal detachment, or posterior capsule opacification (PCO), where the lens capsule becomes cloudy. PCO can be easily treated with a simple laser procedure.
The Future of Cataract Surgery
The future of cataract surgery looks promising, with ongoing advancements aimed at further
enhancing patient outcomes:
Smart IOLs: Research is underway on IOLs that can adjust focus dynamically, much like the natural lens of the eye.
Gene Therapy and Pharmacological Advances: These could potentially delay or prevent the onset of cataracts, reducing the need for surgery.
AI and Robotics: Artificial intelligence and robotic systems may provide even greater precision and personalization in cataract surgery. Conclusion
Modern cataract surgery represents a remarkable achievement in medical science, offering millions of people the chance to regain clear vision with minimal disruption to their lives. With continued innovation and research, the future holds even greater promise for those
affected by cataracts, ensuring that this common condition can be treated with increasing precision, safety, and effectiveness.