The Importance of Early Diagnosis of Autism And ADHD: A Guide for Parents and Caregivers
Introduction
Autism spectrum disorder (ASD) and Attention-Deficit/Hyperactivity Disorder (ADHD) are two
neurodevelopmental conditions that can significantly impact a child’s cognitive, emotional, and
social development. Early diagnosis of these conditions can be a crucial step in providing
appropriate interventions and support. This blog aims to provide parents and caregivers with a
comprehensive understanding of why early diagnosis matters and how to recognize the signs,
and why acting quickly can make a difference in the lives of children with Autism and ADHD.
Understanding Autism and ADHD
Autism Spectrum Disorder (ASD) is a neurodevelopmental condition marked by difficulties in
social communication and the presence of restricted interests and repetitive behaviors. The
term "spectrum" signifies the vast range of severity and symptoms, which can differ
significantly from one person to another. Some children with ASD may exhibit advanced verbal
skills yet find it challenging to grasp social cues, whereas others might have limited or no verbal
communication abilities.[2]
Attention Deficit/Hyperactivity Disorder (ADHD) is on the other hand, refers to a
neurodevelopmental disorder that typically appears in early childhood. ADHD is marked by
ongoing patterns of inattention, hyperactivity, and impulsivity. These behaviors frequently
disrupt daily functioning, making it difficult for children to concentrate on tasks, complete
assignments, and regulate their impulses. ADHD is more commonly diagnosed in boys than in
girls.[1]
The Prevalence and Diagnostic Criteria
The prevalence of ADHD and ASD has been increasing. According to the Centers for Disease
Control and Prevention (CDC), around 6.1 million children in the U.S. have been diagnosed with
ADHD, and approximately 1 in 54 children have been identified with ASD.[5] The diagnostic
criteria for these conditions are based on the Diagnostic and Statistical Manual of Mental
Disorders – Fifth Edition (DSM-V) guidelines.[1] Other diagnostic criteria like
– DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
– DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text
Revision
– ICD-10: International Classification of Diseases, Tenth Revision [3]
are also used.
Recent studies indicate that the global prevalence of ADHD in children and adolescents is 7.6%
for ages 3-12 years and 5.6% for ages 12-18 years. ADHD is more commonly diagnosed in boys
(15%) than in girls (8%), and there are variations in diagnosis rates among different racial and
ethnic groups.[3]
For ASD, the global prevalence is estimated at 0.72%, with U.S. rates showing 3.40% among
children and adolescents aged 3-17 years. ASD occurs across all demographic groups but is
nearly four times more common in boys.[4]
These statistics underscore the importance of early detection and intervention for better
management and support of individuals with ADHD and ASD.[3]
Healthcare Provider’s Role & Early Diagnosis Challenges
Healthcare providers, including pediatricians, psychologists, and developmental specialists, are
vital in diagnosing ADHD and ASD early.[2] They use clinical interviews, behavioral assessments,
and standardized tests.[2] Collaboration with parents, teachers, and caregivers is crucial to
gather comprehensive information about the child's behavior in various settings.[3] Despite
these efforts, early diagnosis can be challenging due to the wide variation in symptoms and the
absence of a definitive test. Cultural and socioeconomic factors also impact recognition and
diagnosis. Healthcare professionals must remain vigilant and use a comprehensive approach to
assessment.
Why Early Diagnosis Matters
1. Improved Access to Support and Interventions: One significant advantage of early
diagnosis for ADHD and Autism is access to tailored interventions and support
programs. Early recognition allows parents to begin behavior therapy, speech therapy,
or occupational therapy, depending on the child's needs.
For Autism, early interventions such as Applied Behavior Analysis (ABA), social skills
training, and speech therapy can improve communication, social interactions, and
adaptive behaviors. Research shows early interventions lead to better long-term
outcomes, making early detection crucial for optimal development.[3]
For ADHD, behavioral interventions manage hyperactivity and impulsivity, while
medication addresses attention deficits. Early educational accommodations, like extra
test time or quiet study spaces, can help.[1]
2. Optimizing Educational Support by family and caregivers: Early diagnosis allows
children to receive essential academic accommodations and support. For ADHD,
structured routines, breaks, and visual aids help maintain focus. Teachers can use
chunking information, graphic organizers, and physical activities to manage excess
energy. For Autism, educational interventions target communication, social skills, and
problem-solving. Special education may offer individualized instruction, sensory-friendly
environments, and assistive technologies. Early support enhances academic
experiences, self-confidence, and motivation, significantly improving long-term
outcomes in social skills, academic performance, and emotional regulation for children
with ADHD and Autism.[6]
3. Educational Planning An early diagnosis enables the creation of individualized education
plans (IEPs) tailored to the child's specific learning needs. This allows schools to
implement accommodations and modifications, helping children with ADHD and ASD
succeed academically.
4. Preventing Secondary Issues Without early diagnosis and intervention, children with
ADHD and ASD face an increased risk of developing secondary issues, including anxiety,
depression, and social isolation. Timely identification and support can help mitigate
these risks and enhance overall well-being.[4]
Recognizing the Signs: Early Warning Signs of ADHD and Autism
Identifying the early signs of ADHD and Autism can be challenging, but there are certain key
indicators to look out for.
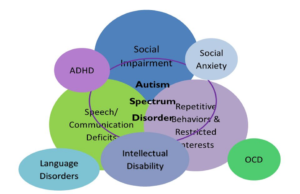
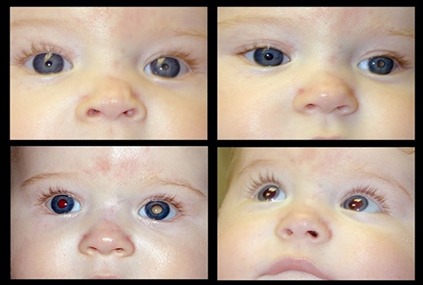
Image curtesy:
https://www.google.com/url?sa=i&url=https%3A%2F%2Fslideplayer.com%2Fslide
%2F8995393%2F&psig=AOvVaw3uXwrb6bfiymMQF2QR1ncb&ust=173217455829
4000&source=images&cd=vfe&opi=89978449&ved=0CBcQjhxqFwoTCLCKrZyz6okDFQAAAAAdAAAAABA7
Autism signs
– Social Communication Issues: Difficulty with eye contact, understanding social cues, or
forming peer relationships.
– Repetitive Behaviors: Engaging in repetitive movements (e.g., hand-flapping) or
insistence on routines and sameness
– Delayed or Abnormal Speech Development: Limited or no verbal communication,
difficulty initiating or maintaining conversations.[2]
– sensory Sensitivities: Overreacting or underreacting to sensory stimuli like light, sounds,
or textures.[3]
ADHD signs
– Inattention: Trouble focusing, following through with tasks, or staying organized.[4]
– Impulsivity: Acting without thinking, interrupting others, or making hasty decisions.[3]
– Hyperactivity: Constant fidgeting, difficulty remaining seated, excessive talking, or
running around.[4]
Conclusion
By recognizing these conditions early, parents can access specialized therapies, educational resources,
and support networks that can significantly enhance a child’s developmental trajectory.[8] Although the
diagnostic process might initially seem overwhelming, it is crucial for understanding the child’s unique
needs and providing the essential tools for their success. The Indian Scale for Assessment of Autism
(ISAA) plays a key role in this, providing a structured framework for evaluating Autism through clinical
assessments and caregiver input.[6] [7]
Reference
1. Antshel, K. M., & Russo, N. (2019). Autism Spectrum Disorders and ADHD: Overlapping
Phenomenology, Diagnostic Issues, and Treatment Considerations. Current Psychiatry Reports,
21(1), 34. https://doi.org/10.1007/s11920-019-1020-5
2. Hours, C., Recasens, C., & Baleyte, J.-M. (2022). ASD and ADHD Comorbidity: What Are We
Talking About? Frontiers in Psychiatry, 13, 837424. https://doi.org/10.3389/fpsyt.2022.837424
3. Salari, N., et al. (2023). The prevalence of ADHD and ASD: A review. Italian Journal of Pediatrics,
49, 48. https://doi.org/10.1186/s13052-023-01456-1
4. Zhong, Q., & Porter, M. (2024). Autism Spectrum Disorder Symptoms in Individuals with a
Primary Diagnosis of Attention-Deficit/Hyperactivity Disorder: A Systematic Review. Review
Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s40489-024-00443-4
5. Centers for Disease Control and Prevention (CDC). (2023). Data and Statistics on Children’s
Mental Health. https://www.cdc.gov/childrensmentalhealth/data.html
6. National Institute for the Mentally Handicapped. (n.d.). Indian Scale for Assessment of Autism
(ISAA) Test Manual. Retrieved from
https://thenationaltrust.gov.in/upload/uploadfiles/files/ISAA%20TEST%20MANNUAL%282%29.
pdf
7. Pedneuroaiims.org. (2020). Indian Scale for Assessment of Autism (ISAA). Retrieved from
https://www.pedneuroaiims.org/pdf-2020/isaa-tool.pdf
8. Dalwai, S., Ahmed, S., Udani, V., Mundkur, N., Kamath, S., & Nair, M. K. C. (2017). Consensus
Statement of the Indian Academy of Pediatrics on Evaluation and Management of Autism
Spectrum Disorder. Indian Pediatrics, 54(5), 385-389. https://doi.org/10.1007/s13312-017-1110-