INTRODUCTION:
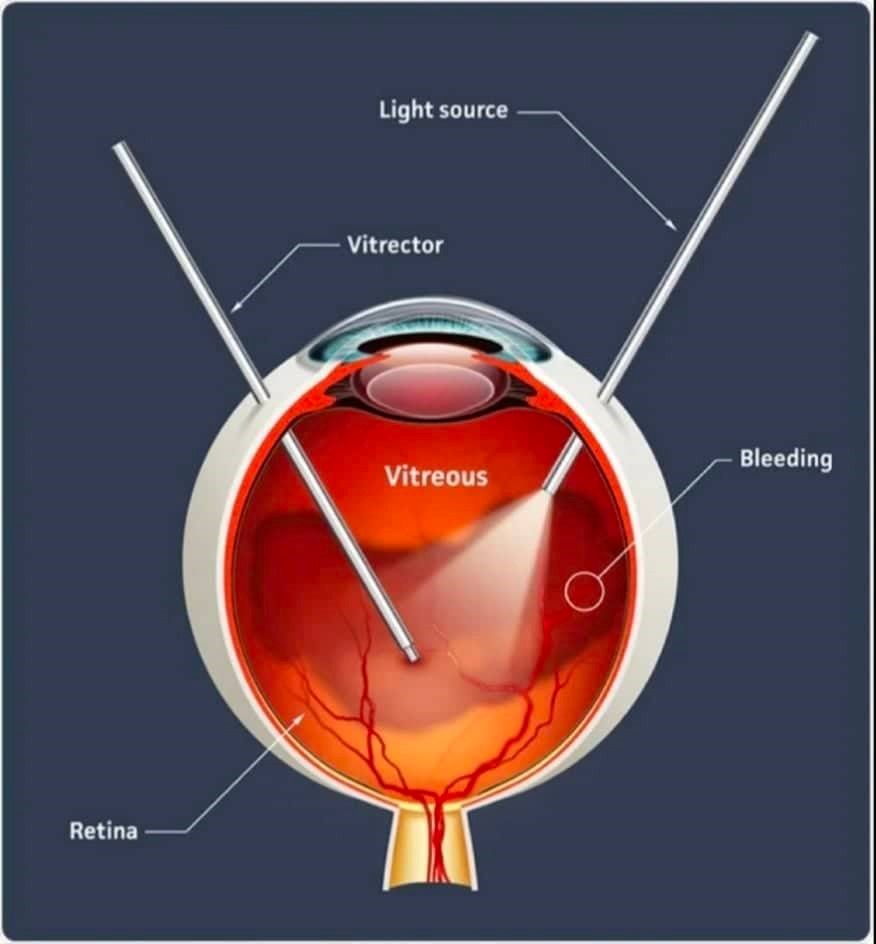
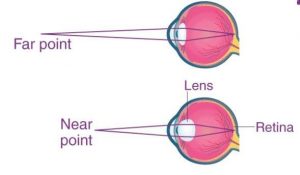
A vitrectomy is a type of eye surgery to treat various problems with the retina and vitreous. During the surgery, removes the vitreous and replaces it with another solution. The vitreous is a gel-like substance that fills the middle portion of eye. Retina is a layer of cells at the back of eye. These cells use light to send visual information to brain. Normally, the vitreous should be clear, so light can pass through the eye and reach the retina.
Certain problems can cause blood and debris to block this light. Scar tissue in the vitreous can also displace or tear the retina. All of this can impair vision.
TYPES OF VITRECTOMY
There are two types of vitrectomy, based on the approach used to remove the vitreous gel; anterior & posterior or pars plana vitrectomy.
- ANTERIOR VITRECTOMY : Anterior vitrectomies are carried out when vitreous gel leaks through the pupil and into the anterior chamber of the eye. Eye trauma, cataracts of the lens, and the corneal or glaucoma surgery can cause this to occurs. Anterior vitrectomies into minimize the risk of developing future problems due to leaking vitreous fluid and to improve visual recovery.
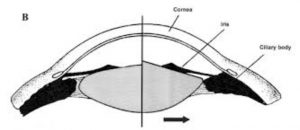
- PARS PLANA VITRECTOMY : Surgical removal of vitreous by aspiration through a needle inserted over the pars plana ciliaris. It is a closed-system technique that uses three ports, placed 3-4 mm posterior to the surgical limbus.
ADDITIONAL SURGICAL STEPS
Membranactomy removal of layers of unhealthy tissue from the retina with minute instruments such as forceps, picks and visco-dissection. It is also called as macular pucker or cellophane retinopathy, epiretinal membrane (ERM) involve growth of the membrane across retina, which interferes with central vision by distorting central retina. ERM is generally related with other disorder like previous retinal tears, branch retinal vein occlusion (BRVO), retinal detachment, uveitis, & central retinal vein occlusion (CRVO).
Fluid/air exchange – injection of air into the eye to remove the intraocular fluid from the posterior segment of the globe while maintaining intraocular pressure to temporarily hold the retina in place or seal off holes in the retina. The air pressure is temporary as the posterior segment will soon re-fill with fluid.
Air/gas exchange: In some cases, gas can be used to help hold the retina in place. Gas, or more typically mixed gas and air, is injected through the sclera and into the posterior segment of the globe. This procedure is often referred to as pneumatic retinopexy. Typical gases used are perfluoropropane or sulfur hexafluoride. The gases are mixed with air to neutralize their expansive properties to provide for a longer acting (than air alone) retinal tamponade. The retinal tamponade acts to hold the retina in place or temporarily seal off holes in the retina. The mixed gases disappear spontaneously once they have accomplished their purpose and the posterior segment re-fills with fluid.
Silicon oil injection – Silicone oil used for long-duration tamponade, is injected into the air-filled vitreous cavity. If perfluorocarbon liquids are used, a direct perfluorocarbon-silicone oil exchange can be performed if the laser has been placed and the buckle has been already tightened.
Photocoagulation– In cases when there is a tear in the retina, or when there are unhealthy damaging blood vessels & it takes place by using the laser to create a microscopic burn in the target tissue. The laser spots are usually applied in 1 of 3 patterns. Before the procedure, you will be given eye drops to dilate the pupils. Rarely, you will get a shot of a local anesthetic. The shot may be uncomfortable.
Scleral buckling – placement of a support positioned like a belt around the eyeball to maintain the retina in a proper, attached position. This is referred to as an “exoplant.” Placement of the Scleral buckle for patients who have had a retinal detachment has been shown to lead to reattachment approximately 80 to 90 percent of the time after one surgery. In cases of failure, most patients are treated with vitrectomy.
Lensectomy – the removal of the crystalline lens through a transscleral retrociliary incision (usually the pars plana) under clinical conditions in which the vitreous gel has to be partially or totally removed.
INDICATIONS:
RETINAL DETATCHMENT
- RD with proliferative vitreoretinopathy
- Giant retinal tears.
- RD with posterior retinal breaks.
- Selected primary RD.
DIABETIC RETINOPATHY
- Non cleaning repeated VH.
- TRD
- Combined RD
- Progressive fibrovascular proliferation.
- Macular distortion by fibrovascular proliferation.
- Macular edema from taut posterior hyaloid.
TRAUMA:
- Traumatic cataract / dislocated lens
- Posterior penetration injuries with VH/RD
- IOFB
- Subretinal membranes/hemorrhage
- Traumatic macular holes
MACULAR SURGERY:
- Macular pucker
- Macular hole
- CNV
- Massive subretinal hemorrhage
- VMT syndrome
- Macular translocation
- Transplantation of photoreceptors or RPE
PEDIATRIC RETINAL DISORDERS:
- ROP
- PHPV
- Familial exudative vitreoretinopathy
- Giant retinal dialysis
- Juvenile RA
- RD secondary to choroidal coloboma
- RD in “morning glory” syndrome/optic disc coloboma
TUMORS:
- Choroidal melanoma
- Complication of retinal angiomatosis
- Combined hamartoma of retina & RPE
- Intraocular lymphoma
- Diagnostic vitrectomy
Complicated anterior segment surgery:
- Dislocated lens fragments
- Dislocated IOL
- Aphakic/pseudophakic CME
- Endophthalmitis
- Choroidal hemorrhage
- Anesthetic needle perforation
UVEITIS:
- Viral retinitis
- Intraocular infections
- Opthalmomyosis
- Inflammatory:
-Bechet’s diseases, sarcoidosis, uveal effusion syndrome
- Pars planitis
- Whipple’s disease
- hypotony
COMPLICATIONS
Vitrectomy procedures are an effective surgery and severe complications are rare. Most surgeries have a 90 percent success rate.
In rare cases, however, complications can occur, especially in immune-compromised individuals and those with a history of eye conditions or surgery.
Possible side effects of vitrectomy procedures include:
- Inflammation or redness, swelling, and pain
- Bleeding inside the eye
- Increased pressure (glaucoma) or reduced pressure in the eye
- Cataract formation or progression of existing cataracts
- Surgical injury, such as a wrong cut or tear, resulting in the need for further corrective surgery
- Swelling of the central part of the retina
change in vision, requiring the need for new eyeglasses
- Loss of night vision, blurriness, or depth perception
- Double vision
- Retinal detachment
- Dislocation or discoloration of the intraocular lens
- Macular pucker or a wrinkle in the retina
Loss of vision
- Allergic reaction or over-reaction to anesthesia, which may risk stroke, heart attack, or pneumonia
RECOVERY: After the surgery, patient eye may be swollen, red, or tender for several weeks. patient might have some pain in the eye and vision may be blurry for a few days after the surgery. He will need 2 to 4 weeks to recover before he can do his normal activities again.