Introduction:
The tear film is a thin fluid layer covering the ocular surface; it is the interface of the ocular surface with the environment. It is responsible for ocular surface comfort, mechanical, environmental and immune protection, epithelial (both corneal and conjunctival) health and it forms smooth, refracting surface for vision. Tear production (about 1,2 microliters per minute, total volume 6 microliters, 16% turnover per minute), evaporation, absorption and drainage are responsible for dynamic balance of the preocular tear film. Homeostatic balance leads to stability of the tear film, that makes possible to realize its functions as lubrication, nutrition and protection of ocular surface. Nonetheless, this stability can be disturb in tear film layers deficiencies, defective spreading of the tear film, in some general diseases and during application of some systemic and/or topical medications and dry eye disease evolves as a consequence of it. These review focused on physiology of the tear film, it’s meaning for the ocular surface stability and analyzed influence of various diseases and conditions on it.
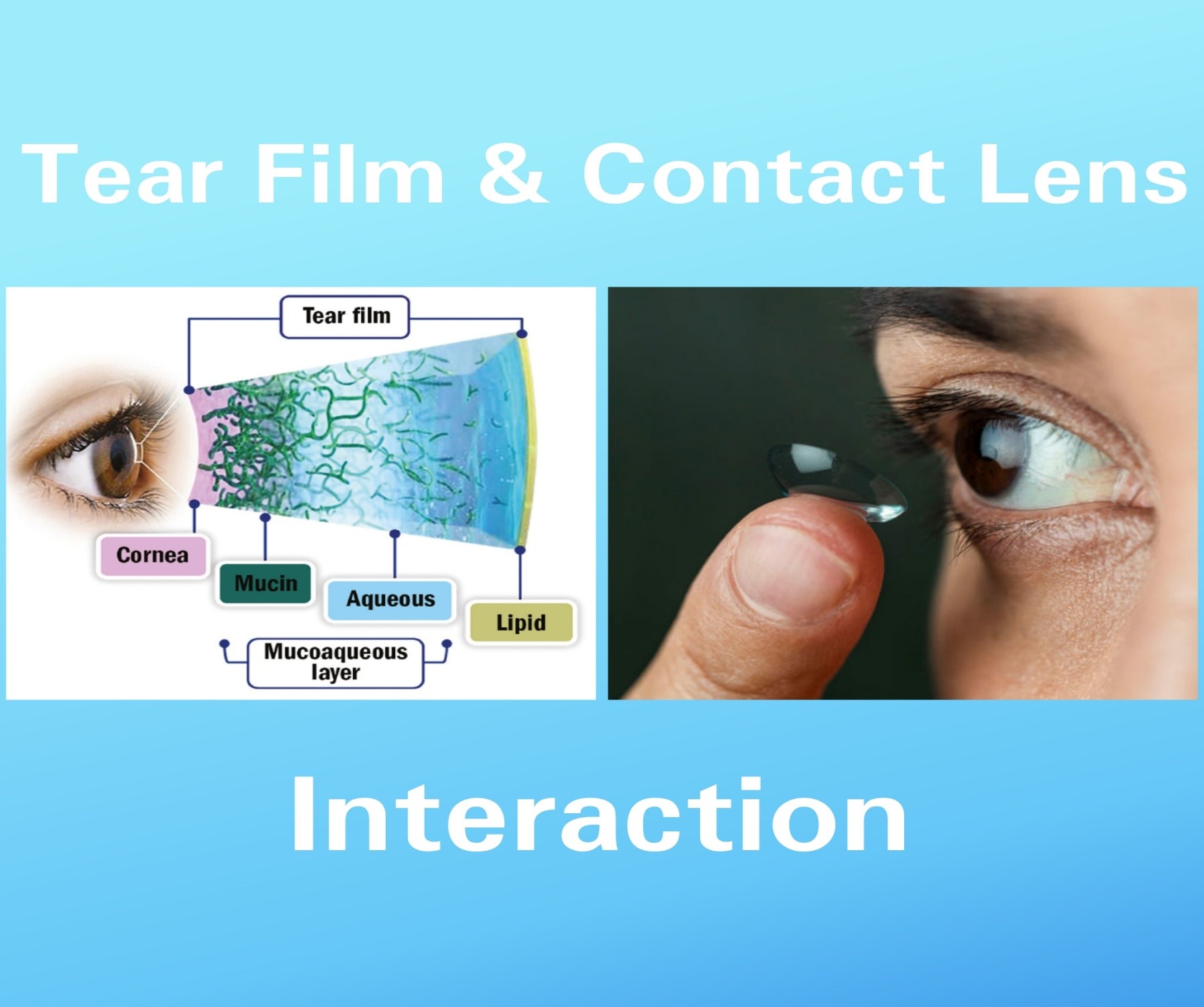
Tear film structure and function:
The traditional description of the tear film is three-layered structure: superficial-oily, middle – aqueous and mucous layer at the base . A more recently proposed model consists of two layers: superficial – lipids and mucin/aqueous glycocalyx gel with decreasing mucin concentration from epithelium to lipid layer. Some authors says, that the tear film is a single unit that acts like a fluid shell.
Tear film layer Function:
A. Lipid layer (meibum)-
• Form the outer layer of the tear film.
• Minimize the evaporation of water from the eye surface
• Isolate ocular surface from the environment
• Improve the stability of tear film
• Provide smooth refracting surface
• Limit contamination of ocular surface from particles(dust) and microorganisms
• Prevent tear contamination by skin lipids
• Limit aqueous layer surface tension
• Counteract tears overflowing onto the skin.
B. Aqueous phase-
• Constitutes roughly 90% of the tear film volume
• Lubricate the ocular surface
• Wash away foreign bodies and contaminations
• Nourish the avascular cornea (oxygen, proteins, inorganic salts)
• Include proteins (lysozyme, lactoferrin, lipocain), immunoglobulins, defensins and glycoproteins responsible for anti-microbial activity
• Include growth factors, vitamins and electrolytes necessary for ocular surface health and epithelial integrity
• Realign corneal microirregularities (refractive properties)
C. Mucous layer:
• Form a glycocalyx over the ocular epithelium that prevents pathogen adhesion
• Bind water to hydrate and lubricate the ocular surface.
• Reduce friction during blinking
• Clear the surface of pathogens and debris
• Contribute to tear stability
• Take part in regulation of epithelial growth
• Might be involved in cellular signaling.
A. Lipids-
The lipid layer is secreted by Meibomian glands, located within tarsal plates of upper and lower eyelids with some small contribution by Moll (modified apocrinic, sudoriferous) and Zeiss (modified subeceous) glands, located within superior and lower eyelids (connected with hair follicles) and possibly epithelial cells. The posterior, aqueous interface consists of polar lipids: ceramides, cerebrosides and phospholipids. The lipid-air interface is formed with nonpolar lipids: cholesterol esters, triglycerides and free fatty acids. The main function of the lipid layer is to reduce evaporation of tears and improve the stability of them. Moreover, the lipid layer provides smooth refracting surface, limits contamination of ocular surface from particles (dust) and microorganisms, prevents tear contamination by skin lipids, limits aqueous layer surface tension and counteracts tears overflowing onto the skin. Regulation of lipid secretion supervenes through modulation of lipid synthesis or cell maturation. The Meibomian gland secretion is a subject of neuronal, hormonal and vascular influences. Androgen, estrogen and progesterone receptors have been identified in adult male and female rats, rabbits and humans. It is suggested that androgens stimulate and estrogens reduce Meibomian secretion. Moreover, Meibomian gland function may be under direct neuronal (predominant parasympathetic, also sympathetic and sensory sources) or indirect vascular (vasoactive intestinal polypeptide VIP) influence to control lipid synthesis and/or excretion.
B. Aqueous component-
The main non-reflex production of aqueous part of mucin/aqueous gel is from the Krauze and Wolfring
glands (accessory lacrimal glands) located in the conjunctiva of superior eye lid and superior conjunctival fornix. The main lacrimal gland is responsible for aqueous tears production secondary to deleterious stimulation and plays important, though not entirely clear role in non-reflecting tearing (dry eye syndrome is noted in patients with damaged main lacrimal gland). The aqueous layer consists of water, electrolytes, proteins, cytokines, vitamins, immunoglobulins and peptide growth factors. Moreover amino acids, bicarbonate, calcium, urea and magnesium were detected in tear film. The aqueous portion of the tear film is responsible for ocular surface lubrication, washing away foreign bodies or
contaminations and nourishing avascular cornea (oxygen, inorganic salts, proteins, glucose). The soluble mucins decrease the surface tension, impact coherence of the aqueous layer, contribute to tear film viscosity [14, 19]. Almost 500 different proteins have been extracted from the tear film. Lactoferrin, lysozyme, lipocalin, secretory immunoglobulin A(sIgA), immunoglobulin G(IgG), immunoglobulin M (IgM), albumin, transferrin, ceruloplasmin, defensins, tear specific prealbumin and glycoproteins participate in the ocular surface antimicrobial activity and defense. Growth factors, vitamins, electrolytes, neuropeptides and protease inhibitors are necessary for retaining ocular surface health and epithelial integrity. Retinol, secreted by the lacrimal gland, is necessary for maintenance of goblet cells and regulates corneal epithelium desquamation, keratinization and metaplasia. The lacrimal gland is affected by both nervous system and various hormones. The gland innervation comes from the first brunch of trigeminal nerve, the facial nerve and sympathetic fibers from the superior cervical ganglion. Stimulation of the ocular surface is the beginning of the main lacrimal gland production (reflexing tearing). The emotional tearing is also connected with this reflex loop. The meaning of the sympathetic part of innervation is thought to stimulate basal tearing but is still not completely understood. The accessory lacrimal glands are heavily innervated, but there is lack of parasympathetic part and most of the innervation is undefined. Androgens and estrogens influence lacrimal gland production. Androgens lack is responsible for reversible degenerative changes of lacrimal gland, decreased volume of the tears, decreased level of proteins in tears. Estrogens remain controversial: some studies described estrogen deficiency linked to keratoconjunctivitis sicca (KCS) and lacrimal gland degeneration, other works have shown no changes in the lacrimal gland and tear film with decreased level of estrogens . Thyroid stimulating hormone (TSH) receptors (present in lacrimal gland) as well as thyroid hormone and tissue interaction are necessary for lacrimal gland secretion. Adequate insulin level is important for lacrimal gland and ocular surface stability and function, because it is necessary for acinar cell and cornea epithelial cell proliferation.
C. Mucins-
The mucous layer of the tear film is produced by both corneal and conjunctival epithelium and the
lacrimal gland and conjunctival goblet cells. It is composed of secreted and transmembrane mucins,
immunoglobulins, salts, urea, glucose, leukocytes, cellular debris and enzymes. Traditional description of the mucins role limits to secreted gel-forming mucins working as lubricating agents and clearing
molecules. Current date indicate its role also as a barrier for corneal and conjunctival epithelium. We
can find two kinds of the mucins: cell surface-associated and secreted. Cell surface-associated mucins
form a thick cell surface glycocalyx, providing through their O-glucans a disadhesive character to the
apical surface of the corneal epithelium. That is why they assure boundary lubrication and prevent
adhesion of corneal epithelium and tarsal conjunctiva during blinking and sleeping. Moreover,
membrane-bound mucins take part in the maintenance of the mucosal barrier integrity to prevent the
penetrance molecules onto ocular surface epithelia. Some recent studies have weighed up membrane-
bound mucins as osmosensors in eukaryotic cells.Secreted mucins have a capability to trap
contaminations (e.g. allergens, debris, pathogens) in order to clearance them from mucosal surface. Gel- forming mucins retaining water, form highly hydrated gel to lubricate ocular surface and reduce shear stress during blinking or rubbing. Moreover, MUC 7 (detected in lacrimal gland), has potent antifungal and antimicrobial activity. Goblet cells may be stimulated for mucin secretion by histamine, antigen, immune complex, mechanical action (i.e. blinking), direct (muscarinic and α-adrenergic receptors on immature goblet cells) and indirect (sensory, sympathetic and parasympathetic innervation of conjunctiva surrounding goblet cells) neural control.