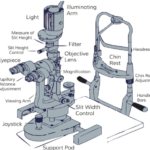
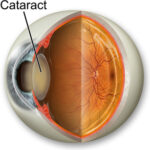
The Potential acuity meter was introduced by Guyton and
Minkowski in 1980. It is a small device that mounts on a slit
lamp and projects on an image of a snellen’s visual acuity
chart , using a 0.15 mm diameter aperture , through clear
areas in the lens on to the retina . A potential acuity
measurement is sometimes appropriate as an estimate of
potential vision prior to a surgical procedure ,especially
cataract surgery . The potential acuity meter is a device that is
designed to project an eye chart directly onto the retina. This
allows the examiner to test the visual acuity without
interference from the cloudy lens. The main purpose of
performing this test is to get an idea of the visual acuity that
the patient can potentially achieve . Prior to committing to
cataract surgery, it helps to know that vision improvement is
possible that means there are no retinal or neurological
problems that will not allow vision improvement despite
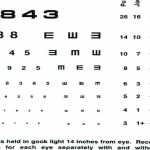
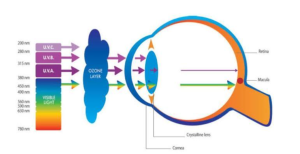
cataract removal . The optical diagram of potential acuity
meter as the beam diverges in the eye, the image of the
snellen’s chart is carried to the retina . A knob on the
Potential acuity meter permits rapid focusing on the letter
chart , using slide scale ranging from +13 D to -10 D. Black
optotypes on a while background create a range of Snellen’s
acuities from 20/20 to 20/400.
Technique of Potential Acuity Meter :-
The test is best performed when pupil is dilated and
dimly lit room, with the PAM mounted on a slit lamp
that is set to the lowest magnification
Glare may be avoided by turning off the illumination .
Other charts should also be turned off or slowed away.
The patient should also wear his or her best spectacle
correction,or trial lenses duplicating the refractive error
should be placed in the instrument .
Amblyopic patient may do better after patching the good
eye . The eye should not be exposed to bright lights prior
to performing the test .
When the patient is ready , the operator should turn the
dioptric setting to the approximate spherical equivalent
of the eye and explain that a light will appear and letters
or numbers will be visible .
Character clarity may change during the test.
The patient is instructed to avoid head movement , as
this will displace the light beam and delay the procedure.
They should report what character are visible through
clenched teeth , minimizing head movement .
The basic set up technique is to focus the beam onto the
patient retina through the cataract .
The patient is encouraged to read the lines of the chart
aloud until no other smaller legible lines are
encountered.
This process is repeated until the examiner is confident
that the patient cannot read any finer lines.
If the patient correctly reads any three characters in a
certain line, then that level of visual acuity is established.
The resulting potential acuity is the smallest line where
the patient was able to read three characters , even if
they lose sight of it an subsequent retesting.
The light beam should be repositioned in other windows
in an effort to enable the patient to see additional finer
lines.
The test takes 5 to 10 minutes per eyes.
Validating the test :-
The PAM has been found to be a very promising
instrument . On reviewing the literature and various
studies conducted on PAM , it has been found that the
PAM correctly predicts the postoperative visual acuity in
patients with moderate cataracts to within three lines on
snellen’s chart in 100% of cases and to within two
snellen’s lines in 91% cases.
The PAM may also erroneously predict improved or
worse vision in eyes with cystoid macular oedema ,
serious detachment of the sensory epithelium of the
macula ,recent postoperative reattached retina ,
geographic atrophy of the retinal pigment epithelium of
the macula , macular hole or cyst ,dense opacities or
glaucoma . However , unlike laser interferometry ,
amblyopia does not appear to interfere with the ability of
the PAM to make accurate predictions.
At times, it may also be difficult to find a clear window
through which to project the fine beam of light with a
dense posterior subcapsular or diffuse cortical changes ,
therefore ,often where we need the information most
,we are least able to estimate retinal acuity.
Disadvantage of Potential Acuity Meter :- Disadvantage of
the Potential Acuity Meter is that it may not always
accurately predict a patient’s actual postoperative visual
acuity. Factors such as corneal irregularities ,media
opacities ,and retinal abnormalities can affect the accuracy
of the results . Additionally , PAM requires a cooperative
patient , which may not always be feasible ,especially in
cases involving chidren or individuals with cognitive
impairments.