Introduction:
Optic neuritis is a condition that affects the eye and your vision. It occurs when your optic nerve is inflamed and swollen. The optic nerve sends messages from your eyes to your brain so that you can interpret visual images. When the optic nerve is irritated and inflamed, it doesn’t carry messages to the brain as well. You can’t see clearly. Optic neuritis can affect your vision and cause pain. When the nerve fibers become inflamed, the optic nerve can also start to swell. This swelling typically affects one eye. But it can affect both at the same time. Optic neuritis can
affect both adults and children of all ages. It’s most commonly seen in white females between the ages of 20 and 40. Loss of vision in optic neuritis commonly reaches its maximum effect within a few days and starts improving within 4 to 12 weeks.
Types of this conditions:
There are three main types of optic neuritis:
A. Typical-This type usually affects one eye only, and most people recover within several days, even without treatment. (But experts still strongly recommend treatment for other reasons.)
B. Atypical- This type usually affects both eyes, and people with it usually don’t recover quickly. Research links it with several other complex neurological (nervous system-related) disorders.
C. Pediatric- This is the childhood form of optic neuritis. While similar to the other two types, there are also some important differences. This form usually has a better overall outlook.
Symptoms :
The following visual problems are common with optic neuritis:
Diminished vision (usually the main symptom)
Trouble distinguishing colors, or noticing that colors aren’t as vibrant as usual
Vision that appears blurry—particularly if it occurs after your body temperature has risen—after you’ve just taken a hot shower or finished a workout, for instance
Inability to see out of one eye
Abnormal reaction of the pupil when exposed to bright light
Pain in the eye, especially when you move it The symptoms of optic neuritis can vary widely in severity. More extensive optic nerve inflammation leads to more noticeable symptoms. Just because you have severe symptoms doesn’t necessarily mean that optic neuritis will never go away. Plus, not everyone who has optic neuritis has problems with their vision. It’s possible for the optic nerve to be inflamed without affecting vision. A careful, medical evaluation of the eye can diagnose optic neuritis even if you don’t have symptoms.
Causes :
The exact cause of optic neuritis is unknown. It’s believed to develop when the immune system mistakenly targets the substance covering your optic nerve, resulting in inflammation and damage to the myelin. Normally, the myelin helps electrical impulses travel quickly from the eye to the brain, where they’re converted into visual information. Optic neuritis disrupts this process, affecting vision. The following autoimmune conditions often are associated with optic neuritis:
Multiple sclerosis. Multiple sclerosis is a disease in which your autoimmune system attacks the myelin sheath covering nerve fibers in your brain. In people with optic neuritis, the risk of developing multiple sclerosis after one episode of optic neuritis is about 50%
over a lifetime. Your risk of developing multiple sclerosis after optic neuritis increases further if an Magnetic resonance imaging (MRI) scan shows lesions on your brain.
Neuromyelitis optica. In this condition, inflammation affects the optic nerve and spinal cord. Neuromyelitis optica has similarities to multiple sclerosis, but neuromyelitis optica doesn't cause damage to the nerves in the brain as often as multiple sclerosis does. Still, neuromyelitis optica is more severe than MS, often resulting in a diminished recovery after an attack compared with MS.
Myelin oligodendrocyte glycoprotein (MOG) antibody disorder. This condition can cause inflammation to the optic nerve, spinal cord or brain. Similar to MS and neuromyelitis optica, recurrent attacks of inflammation can occur. Recovery from myelin oligodendrocyte glycoprotein (MOG) attacks is usually better than recovery from neuromyelitis optica. When symptoms of optic neuritis are more complex, other associated causes need to be considered, including:
Infections. Bacterial infections, including Lyme disease, cat-scratch fever and syphilis, or viruses, such as measles, mumps and herpes, can cause optic neuritis.
Other diseases. Diseases such as sarcoidosis, Behcet’s disease and lupus can cause recurrent optic neuritis.
Drugs and toxins. Some drugs and toxins have been associated with the development of optic neuritis. Ethambutol, used to treat tuberculosis, and methanol, a common ingredient in antifreeze, paints and solvents, are associated with optic neuritis.
Diagnosis:
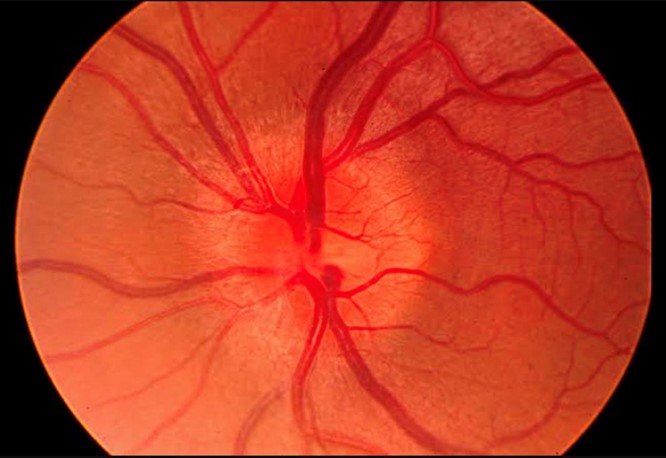
Check to see if your optic nerve is swollen by looking inside your eye with an instrument called an ophthalmoscope.
Test your side (peripheral) vision.
Test to check how well you see colors.
Check to see how your pupils respond to light.
Treatment:
In some cases, you may not need any treatment for optic neuritis. After a few weeks, it may go away on its own and your vision will return to normal. This is more likely if you don’t have another health condition that has triggered the optic neuritis. Sometimes your healthcare provider may recommend a brief course of steroids, usually injected into your vein. These may help your vision improve more quickly and minimize inflammation and swelling. You may also need treatment for another health condition if it’s considered the source of your optic neuritis. If your healthcare provider thinks MS or neuromyelitis optica is causing the condition, they will discuss other diagnostictests and long-term treatment options with you.
Complications:
Taking corticosteroids on a long-term basis can lead to side effects, such as high blood sugar, weight gain, and bone problems, which affect your whole body. Overall, corticosteroids may not lead to a better outcome than letting the condition run its course. But in people with certain brain changes seen on MRI, IV (intravenous) steroids may help prevent future episodes of optic neuritis.