It is an idiopathic esotropia which develops in first 6 months of life in a normal infant without any significant refractive error and limitation of ocular movements. It is also called early-onset, congenital and essential infantile esotropia.
Infrequent periods of convergence are normal up to age of 4 months but thereafter any deviation of the eye is abnormal and must be reported.
Signs
- There is fairly large and stable angle of deviation (more than 30 prism dioptre).
- There is alternating fixation in primary position in most of the infants.
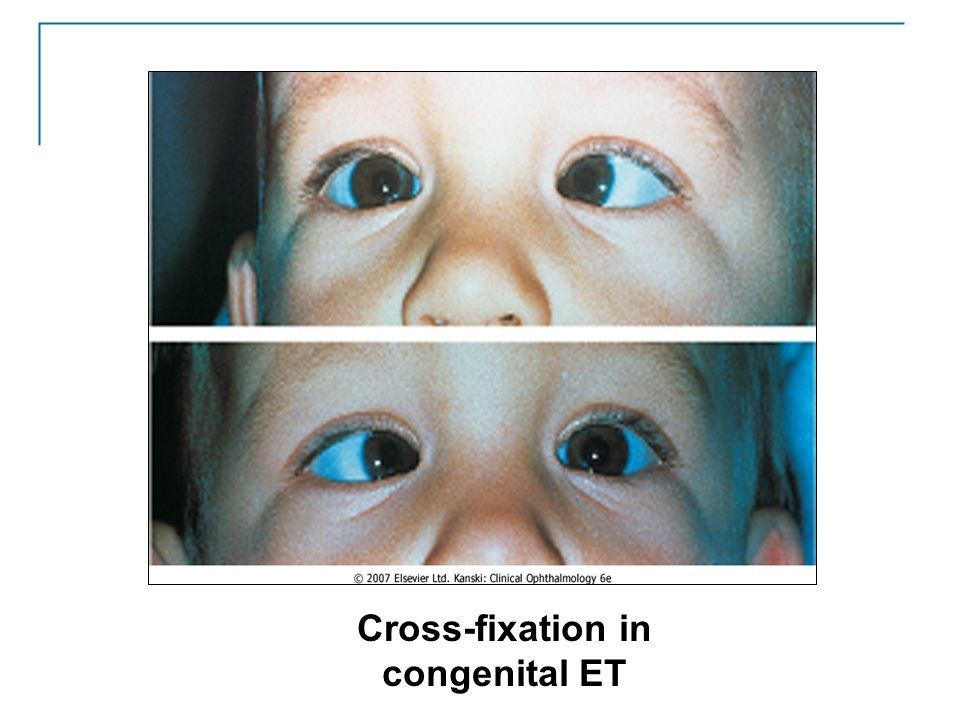
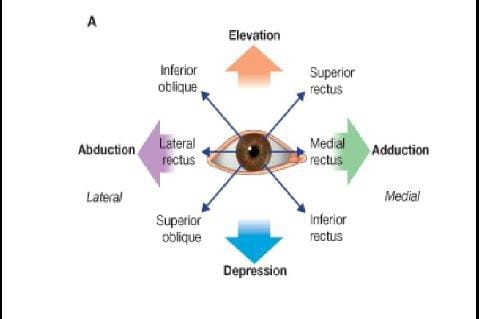
Cross fixation is observed in side gaze i.e child uses left eye for right gaze and right eye for left gaze. It may give the false impression of bilateral deficiency of abduction like 6th nerve palsy. Abduction can be carried out by doll’s head manoeuvre or by rotating the child. If both these fail, monocular patching for few hours will able the eye to abduct.
- Horizontal nystagmus is seen in child and there is asymmetry of optokinetic nystagmus.
- There is refractive error of +1 to +2, which is normal for the age of the child.
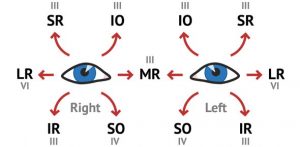
- Over action of inferior oblique (IO) may be present which develops in initial stage or later in life.
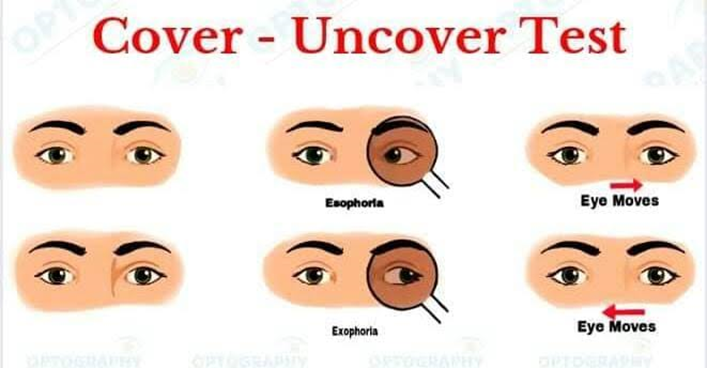
- Dissociated vertical divergence (DVD) is seen in 80% of the children by the age of 3 years. It is manifested by covering one eye. When one eye is covered, it shows up drift with extorsion. When cover is removed, eye goes down without corresponding down drift of other eye, so DVD does not obey Hering law. It is usually bilateral but can be asymmetrical.
Differential Diagnosis
- Bilateral congenital 6th nerve palsy. It is rare and can be excluded
- Secondary ( Sensory esotropia) due to organic eye disease.
- Nystagmus blockage syndrome in which convergence lessens the frequency of horizontal nystagmus. However it shows up in abduction and child adopts a abnormal head posture in the form of face turn in order to maintain fixation and BSV.
- Duane syndrome type 1 & 3.
- Mobius sndrome.
- Strabismus fixus.
Initial Treatment
Initial procedure can be
- Bilateral medial rectus recession OR
- Unilateral medial recession with lateral rectus resection
- Angles larger than 50 degree will require recession of both medial recti as well as resection of one lateral rectus.
- Very large angle may require recessions of 6.5 mm or more, however, recessions of medial rectus musles of more than 6.5 mm have been abandoned as they cause over correction of the deviation.
- Associated significant inferior oblique over action should also be managed at this stage.
- Acceptable goal is alignment of the eyes within 10 prism dioptre.
Early ocular correction provides the best chance of development of binocular single vision. Ideally eyes should undergo alignment procedure by the age of 1 year and very late by the age of 2 years, but it is indicated only after attempt to correct refractive error and amblyopia has been made already.
There is evidence of good sensory outcome and improved binocular function if surgery is done even earlier than12 months.
Subsequent Treatment
Under correction
It may need further recession of both medial rectus muscles, resection of unilateral or bilateral lateral rectus resection or surgery to the other eye. Any plan depends upon the initial procedure.
Inferior oblique over action
It is corrected by
- Disinsertion
- Recession
- Myectomy
Over action may show up subsequently at the age of 2 years. It is unilateral initially but turn out to be bilateral within 6 months. Therefore, parents should be informed that child may need further surgery despite of initial good results.
DVD
Surgical treatment is done owing to psychological reasons for parents satisfaction and is indicated when it is cosmetically unacceptable.
Options include
- Superior rectus recession with or without posterior fixation sutures.
- Resection or tuck of inferior rectus muscle.
- Inferior oblique anterior transposition.
Amblyopia
Preference of monocular fixation commonly develops after surgery which leads to amblyopia or lazy eye. It occurs in about 50% of the cases.
Accomodative element
If eyes are straight after initial surgery and then start to converge again, accomodative factor must be suspected. Therefore, regular refraction is essential.