Fluorescein is a synthetic organic compound available as a dark orange/red powder soluble in water an alcohol.
Fluorescein is a small molecule that is only loosely bound to plasma proteins, for example, only about 65% to albumin, and this small size enables it to leak readily through patent inter endothelial cell junctions.
SYNTHESIS :
It can be prepared from phthalic anhydride an resorcinol in the presence of zinc chloride via the Friedel-Crafts reaction.
Other name – Resorcinolphthalein
FLUORESCEIN IN OPTHALMOLOGY :
- Intraocular dynamic studies (fluorpmetry) tear film drainage studies penetration to anterior segment structures.
- Fluorescein angiography (in acquired macular & retinal vascular pathologies)
- Staining techniques
- Evalution of tear drainage
- Applanation tonometry
Fluorescein Angiography :
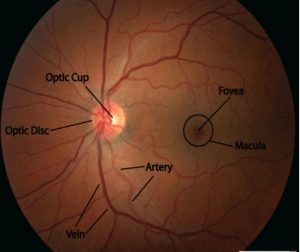
Fluorescein angiography (FA) is when your ophthalmologist uses a special camera to take pictures of your retina. These pictures help your ophthalmologist get a better look at the blood vessels and other structures in the back of the eye.
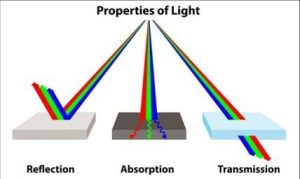
Principle :
A molecule is exited by light of certain wavelength to a higher energy level, released photon then comes down to original state.
2ml of 25% or 5ml of 10%solution
80% protein bound and 20% free into circulation.
What Is Fluorescein Angiography Used for?
FA is often recommended to find and diagnose eye disease including:
- Macular edema (swelling in the retina that distorts vision)
- Diabetic retinopathy (damaged or abnormal blood vessels in the eye caused by diabetes)
- Macular degeneration
- Blockage of veins inside the eye, called BRVO or CRVO
- Macular pucker (a wrinkle in the retina caused by a buildup of fluid behind it)
- Ocular melanoma (a type of cancer affecting the eye)
FA IS ALSO USED TO :
Track changes in eye disease over time
target treatment areas
How Is Fluorescein Angiography Done?
FA is usually done in your ophthalmologist’s office. It often takes less than 30 minutes.
Here is what will happen:
Your ophthalmologist or an assistant will put drops in your eyes to dilate (widen) your pupil.
A yellowish colored dye (fluorescein) is injected in a vein, usually in your arm. It takes about 10–15 seconds for the dye to travel throughout your body. The dye eventually reaches the blood vessels in your eye, which causes them to “fluoresce,” or shine brightly.
SIDE EFFECTS OF FLUORESCEIN :
Temporary yellowing, orange yellow urine.
Nausea , vomiting,urticaria, toxic neuritis, local tissue necrosis, extravasation into skin, vasovagal reactions.
Hypofluorescence : 1. Vascular filling defefcts
2. Blockage by heamorrhage RPE hypertrophy
Hyperfluorescence: Leakage
Pooling
Staining
Transmission (window defect)
STAINING TECHNIQUES :
fluorescein eye stain :
This is a test that uses orange dye (fluorescein) and a blue light to detect foreign bodies in the eye. This test can also detect damage to the cornea. The cornea is the outer surface of the eye.
How the Test is Performed?
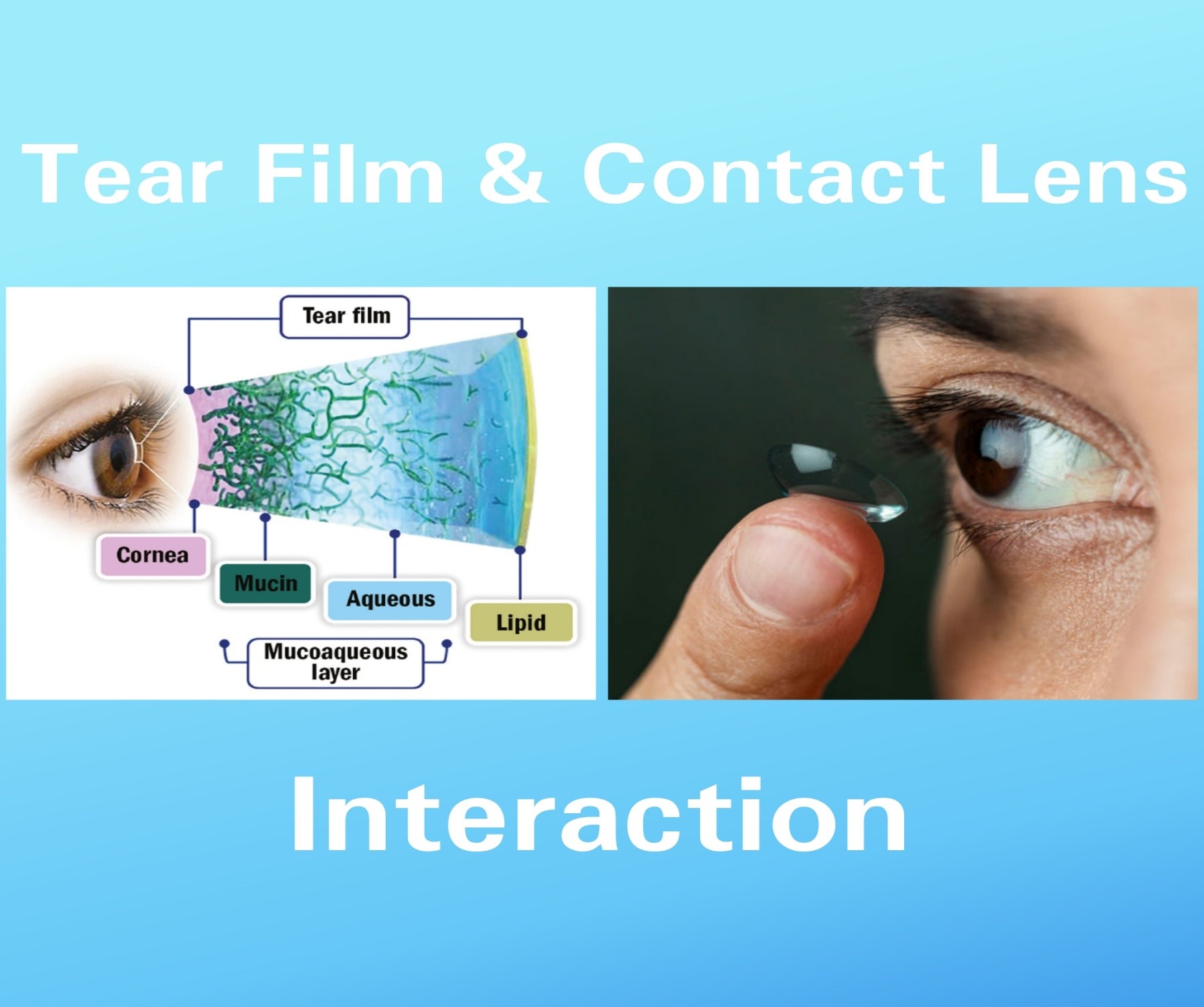
A piece of blotting paper containing the dye is touched to the surface of your eye. You are asked to blink. Blinking spreads the dye and coats the tear film covering the surface of the cornea. The tear film contains water, oil, and mucus to protect and lubricate the eye.
The health care provider then shines a blue light at your eye. Any problems on the surface of the cornea will be stained by the dye and appear green under the blue light.
TEST FOR DRY EYE :
TEAR BREAK UP TIME :
Tear break-up time (TBUT) also known as tear film break-up time (TFBUT) is the time taken to appear first dry spot on cornea after a complete blinking. TFBUT measurement is an easy and fast method used to assess the stability of tear film. It is a standard diagnostic procedure in the dry eye clinics. The volume of tear in the eye depends on two factors, drainage through the lacrimal passages and evaporation. Factors like decreased tear production, increased evaporation rate, tearfilm instability, tear hyperosmolarity, inflammations, ocular surface damages etc. can cause dryness to the eyes.
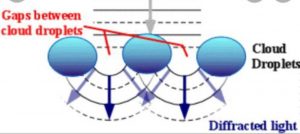
Conventional and most common TBUT measurement method is using slit lamp and sodium fluorescein. Noninvasive instruments are used for automatic non-invasive tear breakup time (NIBUT) measurements.In non invasive procedure, a grid or concentric ring pattern is projected onto cornea and patient is asked to blink. the rings will appear distorted when cornea becomes dry. Tearscope is a commercially available instrument used to measure NIBUT.
TEST FOR LACRIMAL DRAINAGE :
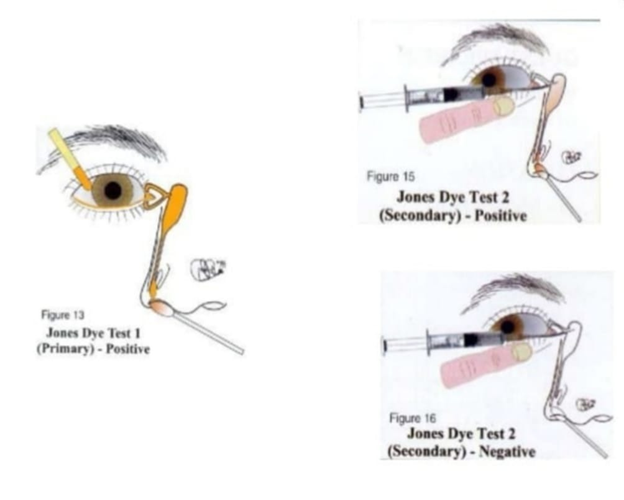
JONES DYE TEST:
- To distinguish between anatomical and functional outflow problems.
- Instill one drop of fluorescein into the conjunctival sac
- Put a cotton bud soaked in anesthetic in the inferior meatus
- If flurorescein is detected after five minutes the system is patient (positive primary Jones Test).
- No fluorescein – Negative Primary Jones Test and the functional obstruction could be anywhere from the punctum to the Valve of Hasner.
- Next, wash the excess fluorescein from the conjunctival sac and syringe.Fluorescein detected, entered the sac – Positive Secondary Jones Test and functional obstruction of the nasolacrimal duct.
If no dye after syringing, Negative Secondary Jones Test, because flurescein not entered the sac and thus, there is stenosis of the puncta or canalicular system – anatomical obstruction.
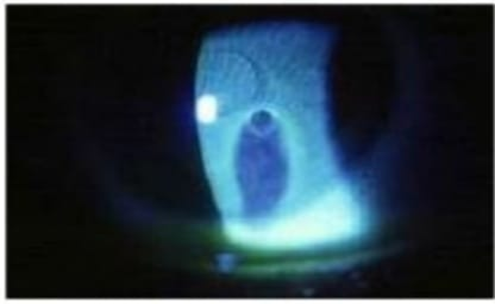
APPLANATION TONOMETRY :
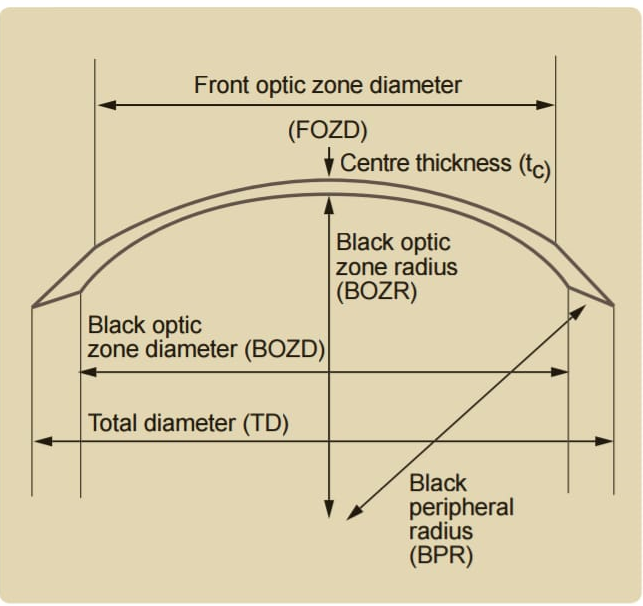
The intraocular pressure is inferred from the force required to applanate a constant area of the cornea, as per the Imbert – Fick law.
- Anasthetic & fluorescein instilled in conjunctival sac
- With cobalt blue filter, brightest illumination and prism advanced until touches apex of cornea
- A pattern of 2 semicircles one above, other below the horizontal midline
- Dial is rotated to align inner margins of semicircles to just touch each other
- Reading on dial multiplied by 10 = Intraocular pressure (IOP).