Diabetes, a chronic condition characterized by high blood sugar levels, has
widespread effects on the body. While most people are aware of its impact on organs
like the heart, kidneys, and eyes, one area that often does not get as much attention is
the cornea. The cornea is the transparent, dome-shaped surface that covers the front of
the eye. For individuals with diabetes, changes in the cornea can have significant
implications for vision and overall eye health.
Let us explore how diabetes affects the cornea, the underlying mechanisms, potential
symptoms, and what diabetic patients can do to manage eye health.

The Relationship Between Diabetes and the Eyes
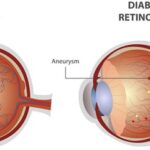
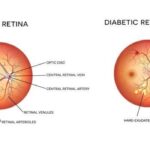
The relationship between diabetes and the eyes is multifaceted. Chronic high blood
sugar can lead to various ocular conditions, including diabetic retinopathy, cataracts,
and glaucoma. However the cornea is often overlooked in this discussion. The cornea
is made up of layers that must remain healthy and hydrated to maintain proper vision.
Diabetes can disrupt this delicate balance in several ways, often leading to changes
that affect vision quality and comfort.
Impact of Diabetes on Corneal Health
1. Corneal Nerve Damage
One of the most significant impact of diabetes on the cornea is nerve damage. The
cornea is rich in sensory nerves, which are responsible for detecting sensations like
touch and pain. These nerves also play an essential role in maintaining the health of
the cornea by helping regulate tear production and coordinating immune responses.
High sugar levels over time can cause diabetic neuropathy, which can damage the
nerves in the cornea. This can lead to a condition called corneal hypoesthesia—a
reduction in corneal sensitivity. As a result, the cornea may not receive the same
protective cues it normally would, making it more vulnerable to injury, infection, and
dryness.
2. Dry Eye Disease
Diabetes is a known risk factor for dry eye disease, a condition where the eyes do not
produce enough tears or the tears evaporate too quickly. The cornea relies on a stable
tear film to keep its surface moist and healthy. Without sufficient moisture, the
corneal cells may become irritated, and over time, the integrity of the corneal tissue
could deteriorate. Dry eye disease is not only uncomfortable but can also cause
blurred vision and increase the risk of corneal ulcers or infections, which could lead to
more severe vision loss.
3. Changes in Corneal Thickness
Another way diabetes affects the cornea is through changes in its thickness. Research
has shown that individuals with diabetes tend to have an increased corneal thickness
compared to those without diabetes. This thickening of the cornea is believed to be
related to the accumulation of excess glucose in the eye tissues. Changes in corneal
thickness can distort the shape and clarity of vision. The cornea’s refractive properties
may also change, contributing to issues such as blurry vision or a fluctuating
prescription for glasses or contact lenses.
4. Corneal Edema
Corneal edema occurs when excess fluid accumulates in the cornea causing swelling.
This condition is particularly common among diabetic individuals especially those
with poorly controlled blood sugar levels. The swelling can cause the cornea to
become opaque, impairing light transmission and leading to blurred vision. Corneal
edema is often exacerbated by other diabetes related issues like diabetic retinopathy or
cataracts, making it more difficult to manage and treat.
Symptoms of Corneal Issues in Diabetic Patients
While not all patients with diabetes will experience corneal problems, those who do
may experience a range of symptoms. These can vary depending on the severity of the
condition but often include:
Blurred or fluctuating vision: The most common symptoms that often signals
corneal involvement.
Dry, itchy, or burning eyes: Indicative of reduced tear production and poor
lubrication of the cornea.
Pain or discomfort: Due to reduced sensitivity or nerve damage.
Frequent eye infections or ulcers: An increased risk of eye infections as the
cornea’s ability to heal and protect itself is compromised.
Sensitivity to light: The cornea may become more sensitive to bright lights due
to swelling or nerve damage.
Importance of Blood Sugar Control
One of the most effective ways to reduce the risk of corneal complications is to
manage blood sugar levels effectively. Keeping blood glucose levels in check helps to
reduce the incidence of nerve damage, minimize the risk of corneal edema and
prevent the formation of other diabetic eye diseases. Regular monitoring of blood
sugar levels, adherence to prescribed medications, and maintaining a balanced diet
rich in nutrients can all contribute to better overall eye health.
Additionally, diabetic patients should undergo regular exams with an ophthalmologist
or optometrist. Comprehensive eye exams can detect early signs of corneal changes,
allowing for prompt intervention. The doctor may also conduct tests to assess corneal
sensitivity, and hydration, providing a clear picture of the corneal health.