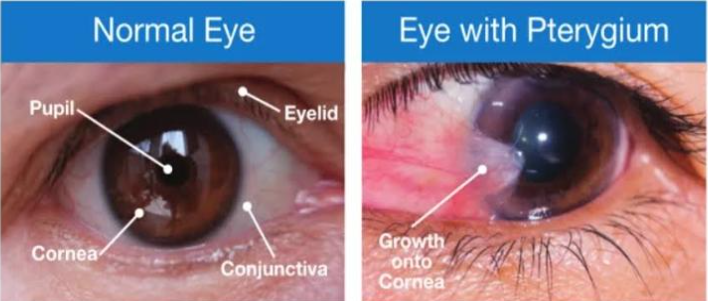
Pterygium is a relatively common ocular surface disease. The clinical aspects and the
treatment options have been studied since many years ago, but many uncertainties still
exist. The core pathologic pathway and the role of heredity in the development of
pterygium are still attractive fields for the researchers. The role of pterygium in corneal
irregularities, in addition to the refractive properties of pterygium removal, has been
increasingly recognized through numerous studies. The association between pterygium
and ocular surface neoplasia is challenging the traditional beliefs regarding the safe
profile of the disease. The need for a comprehensive clinical classification system has
encouraged homogenization of trials and prediction of the recurrence rate of the
pterygium following surgical removal. Evolving surgical methods have been associated
with some complications, whose diagnosis and management are necessary for
ophthalmic surgeons. According to the review, the main risk factor of pterygium
progression remains to be the ultraviolet exposure. A major part of the clinical
evaluation should consist of differentiating between typical and atypical pterygia, where
the latter may be associated with the risk of ocular surface neoplasia. The effect of
pterygium on astigmatism and the aberrations of the cornea may evoke the need for an
early removal with a purpose of reducing secondary refractive error. Among the surgical
methods, conjunctival or conjunctival-limbal autografting seems to be the first choice for
ophthalmic surgeons because the recurrence rate following the procedure has been
reported to be lower, compared with other procedures. The use of adjuvant options is
supported in the literature, where intraoperative and postoperative mitomycin C has
been the adjuvant treatment of choice. The efficacy and safety of anti–vascular
endothelial growth factor agents and cyclosporine have been postulated; however, their
exact role in the treatment of the pterygium requires further studies.
Epidemiology-
Depending on the population studies, the prevalence of pterygium lies within the range
of 1% to more than 30%.According to a meta-analysis of 20 studies published in 2015,
the pooled prevalence of pterygium is around 10%. The maximum prevalence rate for
pterygium has been reported in a Chinese study on rural population, where a rate of
33% was yielded.
Some reported risk factors for pterygium are age,male sex, experience of outdoor
job,low education, rural residence, low income, darker skin complexion, and
smoking.In a North American study, the prevalence of pterygium was reported to be
2.5–3 times higher in Black population compared with Whites. Despite its worldwide
distribution, pterygium is the most common in geographic latitude 40° around the
equator. The prevalence rate of pterygium within this area is reported to be more than
10 times higher than that outside it, which strongly supports the role of ultraviolet (UV)
irradiation in the pathogenesis of pterygium.
Pterygium complications-
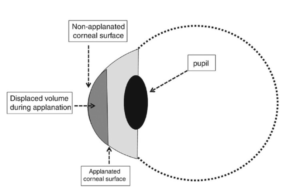
A. Corneal astigmatism-
Although physical obscuration of the visual axis by pterygium is an absolute indication
for surgical intervention, the visual function of the patient may be affected far earlier in
the course of the disease, persuading the ophthalmologist to intervene before reaching
the end stage. Pterygium can have a noteworthy impact on the corneal surface
regularity indices through inducing astigmatism and surface asymmetry.Pterygium
usually results in a with-the-rule astigmatism due to the flattening of the horizontal
meridian along its leading head.The formation of a tear meniscus between the corneal
center and the pterygium apex has been proposed for the underlying mechanism of
horizontal corneal flattening. The change of corneal curvature caused by pterygium
cannot be evaluated by refraction or conventional keratometry because this change
occurs over the nasal paracentral cornea in the horizontal meridian. Therefore,
computerized videokeratography seems to be the best tool in evaluating corneal
topographic changes in pterygium patients.It is now believed that topographical
changes induced by pterygium are almost always reversible following pterygium
removal. However, pterygium-induced astigmatism should be evaluated through a
reliable approach to predict the impact of pterygium removal on the visual function.
Based on the preoperative refractive error, the residual postoperative astigmatism may
be predicted through some proposed equations; however, ophthalmologists should
always be cautious about using mathematical formulas in real-world clinical situations.
The following equation is an example:
Postoperative refractive cylinder = 0.283 + 0.266 × preoperative refractive cylinder.
Larger pterygia are believed to induce higher refractive errors, and their removal is
associated with more significant changes in corneal topography. Lin and Stern reported
that pterygium induces significant astigmatism when it exceeds beyond 45% of the
corneal radius. Tomidokoro and colleagues suggested the percentage extension of
pterygium on the cornea as a predicting factor for the degree of corneal irregularity.
They proposed the following equation to express the relationship:
Induced corneal changes by pterygium (D) = 0.097 × pterygium extension − 1.028.
Similarly, Hochbaum and colleagues postulated that the pterygium-associated corneal
astigmatism can be calculated via a predictive model using horizontal extension of
pterygium and resultant tractional force exerted onto the cornea. Oner and colleagues
reported that both the length and width of pterygium are responsible for pterygium-
induced astigmatism. Mohammad-Salih and colleagues demonstrated that pterygium
can induce an astigmatism of more than 2 D when its total area is ⩾6.2 mm2. In a
recent study, multivariate analysis revealed that two parameters, vascularity and
horizontal length, influence the degree of astigmatism induced by the pterygium.
Accordingly, to increase the reliability of the prediction model, the authors added
vascularity index to the regression equation:
Pterygium-induced astigmatism = 0.080 × RL (%) + 0.039 × VI – 0.823,
where RL is the length of pterygium divided by the corneal horizontal diameter and VI
stands for vascularity index which is determined through an anterior segment
photograph using computerized algorithms.
The correlation between pterygium advancement and the increase in corneal irregularity
was proved in a recent study on 456 eyes. In this study, the Fourier harmonic analyses
for a series of data revealed the precedence of topographical irregularity due to
pterygium pregression.
The effect of pterygium on the high-order aberrations of the cornea has also been
described. Through the analysis of Placido disk data or anterior segment OCT outputs,
it has been revealed that exacerbation of high-order aberrations due to pterygium
progression alters with the size of the pterygium and diameter of the analysis.In a recent
study, it was shown that significant high-order aberrations were induced in 5.0-mm
diameter when the head of the pterygium exceeded 25% of corneal diameter. 107 Initial
findings assumed that the third-order aberration is mostly induced by the pterygium,
while the contribution of the high-order aberration is relatively small. It is currently
believed that contributions of the coma and coma-like aberrations are the highest,
followed by the spherical-like aberration. Such an association has not been observed in
the spherical aberration. Minami and colleagues showed that when the pterygium size
was more than 45% and 40% of the corneal diameter, the coma-like and spherical-like
aberration significantly increased, respectively. In contrast, there was no increase in the
spherical aberration. Anterior segment optical coherence tomography (AS-OCT) and
Zernike analysis may facilitate objective grading of pterygium progression based on
changes in corneal optics.
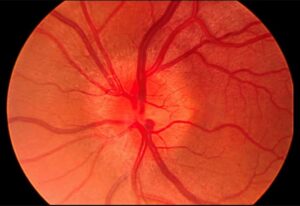
B. Ocular surface squamous neoplasia-
OSSN refers to a spectrum of ocular surface conditions ranging from mild dysplasia to
invasive SCC. There are same risk factors for OSSN and pterygium, so these two
conditions can coexist or are even related. These common risk factors include UV
radiation, chronic inflammation, chronic exposure to ocular surface irritants (such as
dust), and oncogenic viruses (such as HPV).Two studies from Australia and three
studies from North America have evaluated the coexistence of OSSN and pterygium in
pathological studies of surgically removed pterygia. OSSN was present in nearly 10% of
pterygium samples in Brisbane and in 5% of cases in Sydney, Australia. In the studies
from North America, the prevalence of the coexistence of OSSN and pterygium has
been reported to be less: around 2% in Montreal, less than 2% in Florida, 113 and 0% in
Toronto. This discrepancy observed in studies is attributable to variations in UV
exposure across geographic regions. It is possible that pterygia diagnosed in regions
with high UV exposure are more susceptible to carry neoplastic features. Another factor
that confounds the prevalence of atypia associates with pterygium is the criterion used
for surgical removal by different studies.Older age and inferiorly located pterygia are two
factors reported to be associated with higher prevalence of OSSN in pterygium
samples.On the contrary, Kao and colleagues reported no significant difference in the
average age of patients with pterygium associated with OSSN and patients having
pterygium without OSSN. They concluded that age is not a significant risk factor for the
development of OSSN in pterygium cases.Hirst and colleagues reported no case of
recurrence after pterygium removal in their samples of simultaneous OSSN and
pterygium, while a recurrence rate of 11% at 1 year was reported for the pterygia
associated with OSSN in the Florida study. It is as same as the recurrence rate reported
for OSSN not associated with pterygium, which is around 12%. Most OSSN cases in the
Florida and Montreal studies were found to have corneal intraepithelial neoplasia (CIN)
I, while CIN II was the most frequent neoplasia in the Australian cases. It may also be
justified in part by the higher UV exposure in Australia, which may cause a rapid lesion
progression.
C. Symblepharon.
D. Corneal scars.
E. Scleral melts.
Conclusion-
The main risk factor for the development and progression of pterygium remains to be
UV exposure. The role of viral agents and the heredity have been suggested, but the
literature lacks reliable conclusions. In addition, these hypotheses have neither changed
the practice, nor presented additional prophylactic and treatment options. Pterygium
should be considered as a diffuse ocular surface disease, and concomitant conditions
such as dry eye should be addressed. The cells responsible for the development of the
pterygium are altered limbal stem cells, and stromal changes are involved in the
progression of the disease. As the altered stem cells are mainly located in the head of
the pterygium, complete removal of the apex is critical in the surgical excision of the
pterygium. The clinical examination of a patient with pterygium should be given more
importance than the past, as atypical features and secondary corneal irregularities may
justify earlier surgical intervention. Association of pterygium with ocular surface
neoplasia has been reported in several studies. Pterygium may induce both astigmatism
and high-order aberrations of the cornea, where the amount of both are correlated with
the size of the pterygium. Surgical removal of the pterygium can reduce the corneal
irregularities, giving a refractive value to an earlier surgical intervention. Also, a
pretreatment classification based on the size, texture, and vascularity of the pterygium
may provide a prediction for the postoperative recurrence rate. It is recommended that
excised pterygia, particularly in atypical cases, be sent for histopathologic studies. The
procedure most advised for the repair of the surgical site is conjunctival and
conjunctiva-limbal autografting, and the use of adjuvant intraoperative MMC seems to
be more effective than other adjuvant options to reduce the risk of postoperative
recurrence. The application of CsA and bevacizumab in the site of excised pterygium
has been reported to be safe; however, reports on the efficacy of these adjuvant
treatments are still inconclusive.