Abstract
Convergence spasm (CS) is a rare disorder characterized by an involuntary state of convergence, miosis, and accomodation secondary to disconjugate gaze. It is a condition that occurs in younger patients and mostly arises from non-organic causes such as hysteria or conversion disorder.
Etiology
1.Functional causes : It has been reported that in most of the cases, convergence spasm is functional in origin. It occurs in patients with hysteria or neurosis.
2.Organic causes: Rarely convergence spasm may be secondary to some underlying organic lesion. It has been reported to occur after head trauma, encephalitis, tables, pituitary adenomas, posterior fossa neurofibroma and Arnold-chiari malformation.
Clinical Issues
In most of the cases, the condition is episodic. In between the attacks, patient are normal. During the episode of convergence spasm, a patient may exhibit following clinical features :
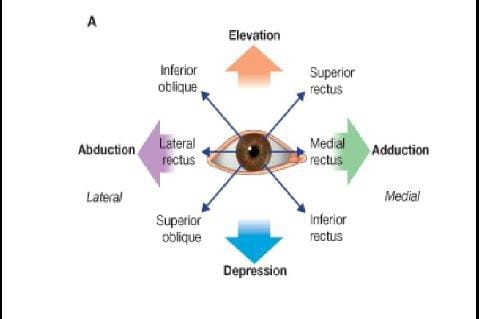
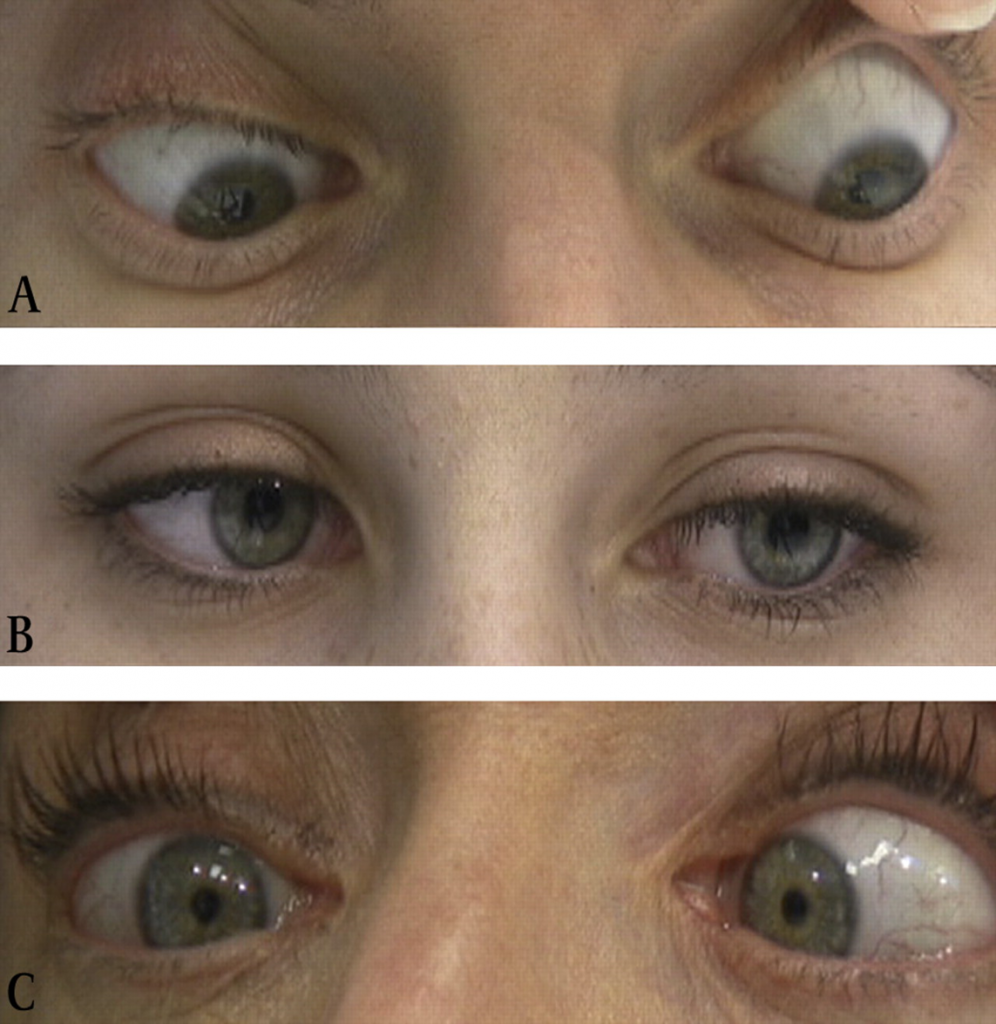
1.Extreme convergence : Eyes may be fixed in a position of extreme convergence resembling bilateral abducens palsy.
2.Homonymous diplopia may be experienced. Patient may give history of intermittent diplopia.
3.Blurring of vision : During the attack, patient may have blurred vision for near due to associated spasm of accommodation. Patient may come with a complaint of difficulty in reading.
4.Miosis: pupils usually become myotic, as a part of near reflex.
5.Induced myopia to the tune of 6D has been reported due to associated spasm of accommodation. Thus during the attack, patient may also have a reduced distance visual acuity.
Psychiatric examination may reveal the underlying hysteria and neurosis in many cases.
Management
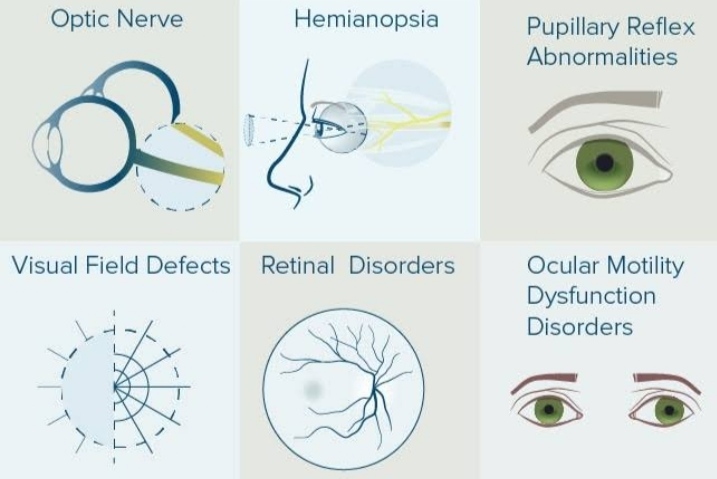
Neurological evaluation : Organic lesions are a rare cause of spasm of convergence, however, each patient should undergo detailed neurological evaluation to rule out associated condition, if any.
Treatment of functional spasm of convergence includes:
1.prolonged atropinization with plus lenses in lower segment of bifocals for near work may be required to break the cycle.
2.Alternate monocular occlusion may be considered as an alternative to atropinization.
3.Psychiatric work-up and therapy is useful as a long-term measure.
Convergence Spasm in Wernicke Encephalopathy.
Three case report of convergence spasm below
Case 1
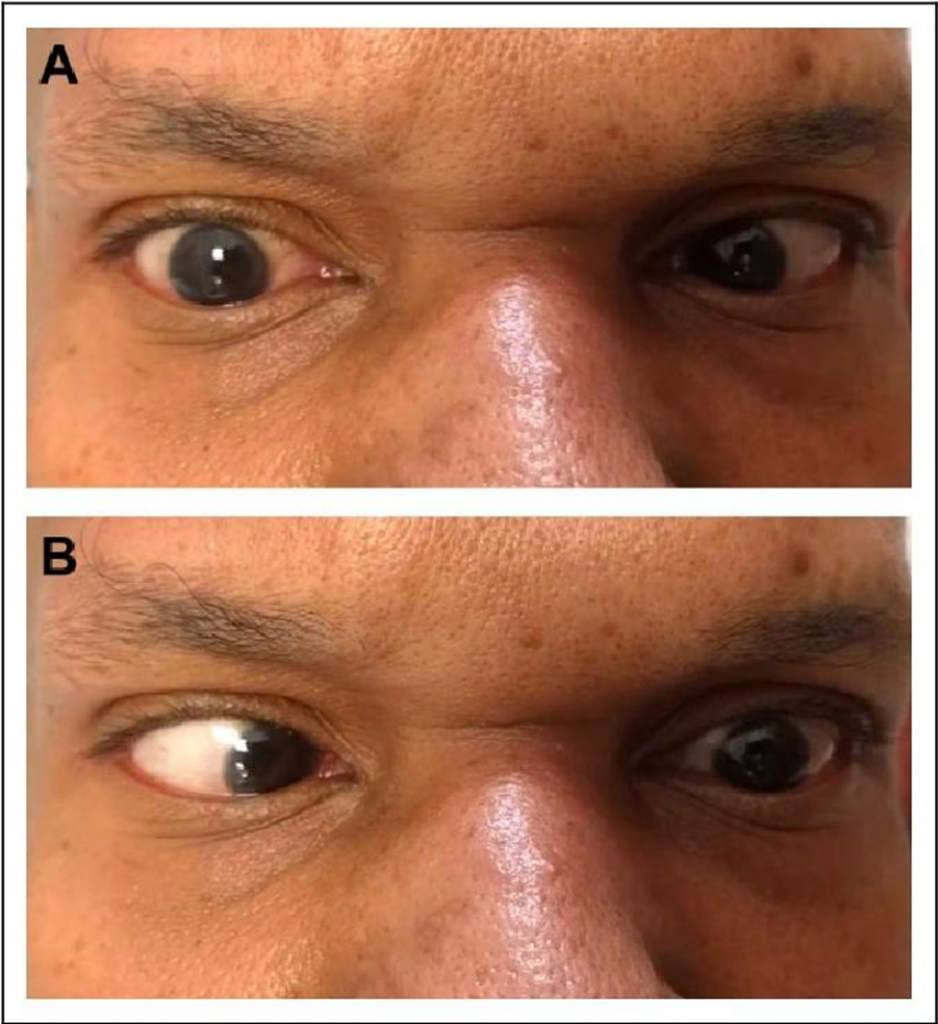
Male/46yrs old
Past History : TIAs, cluster headache & gastric bypass
Presented with : sudden onset right sided headache, diplopia, righ-sided ptosis and hemiplegia.
Examination : Functional ptosis, bilateral pseudoabducens palsy, restricted up-gaze & collapsing weakness.
Bloods: Normal (including AchR antibodies).
MRI Brain : Mild small vessel ischemia.
Infrared video: convergence spasm
Case 2
Female /48yrs old
Past History : Acute sensory axonal neuronopathy
Presented with : Variable fatigue, diplopia, sphincteric disturbance, generalised weakness and ataxia.
Examination : Inconsistent (normal vs. INO)
Bloods : Ganglioside & Ach R Abs negative
NCS and MRI Brain : Normal
Infrared video : Convergence Spasm
Case 3
Male / 16yrs old
Past History : Nil significant
Presented with : Episodes of diplopia with sustained convergence of right eye lasting less than 24 hours without associated symptoms.
Examination :
Between episodes : normal
In clinic : pseudoabducens palsy
MRI BRAIN : Normal
Infrared video : Flickers of convergence with pupillary construction.
Conclusions
Convergence Spasm is:
- Difficult to observe and easy to misinterpret.
- Often an expression of functional disease.
- Often the stimulus for expensive /invasive / unhelpful investigation
Infrared video goggles allow :
Observation of eye movement under controlled conditions & video play back
Technique not previously used for this purpose.
These case reports demonstrate potential for this diagnostic technique.
&
When the symptoms do not fulfil diagnostic
Criteria of a neurological disorder, the objective
Examination is not neurologically congruous and
There is not consistent response to an appropriate
Treatment, a psychological condition should be
Actively searched for Infrared video goggles.
Discussion
Spasm of the near reflex is a disorder characterised by intermittent Episodes of convergence, miosis and accommodation. It may mimic Bilateral and sometimes unilateral nervus abducens paresis. The Patient complains of double vision or blurred vision. Prominent Miosis on convergence is the clue in differentiating convergence Spasm from true organic causes of convergence phenomena.Spasm Of the near reflex as described above may rarely occur in patients with Organic disorders, but is more commonly psychogenic.
Spasm of the near reflex is one cause for esotropia. Organic dis-Orders causing esotropia include conditions such as abducens palsy, Tonic convergence spasm (part of dorsal midbrain syndrome), pons Lesions in multiple sclerosis, myasthenia gravis and Wernicke’s Encephalopathy. Patients with functional spasm of the near reflex Have associated somatic complaints and behavioural abnormalities. Blepharoclonus (frequent blinking), poor co-operation in other Motor tasks and tunnel vision may occur. The patient has a full range Of eye movement with pursuit of own hand and with one eye covered. Normal optokinetic nystagmus is observed.