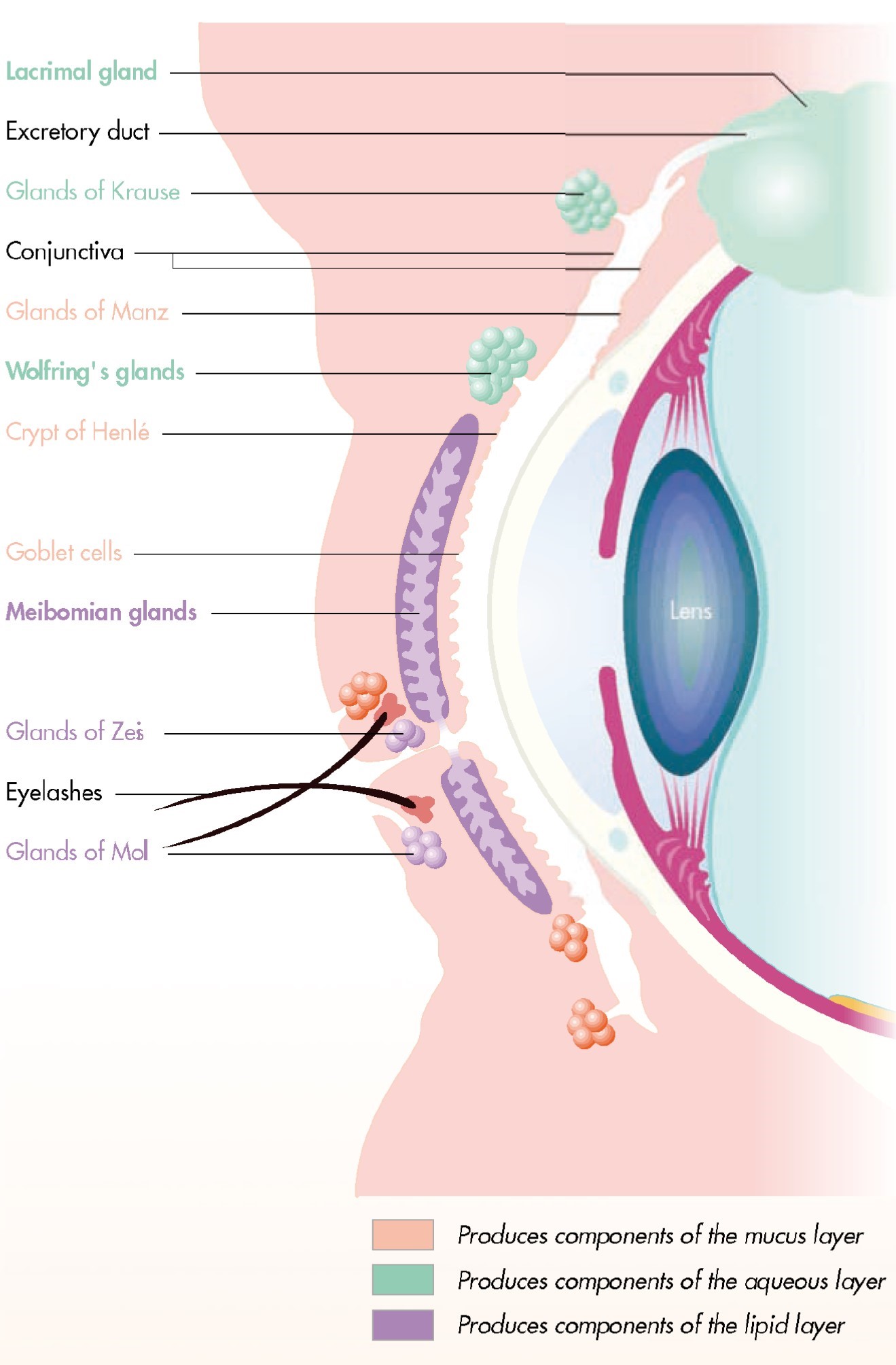
The conjunctiva contains two types of Glands:
The mucin secretary glands ( goblet cells, crypts of Henle, glands of Manz ) and the accessory lacrimal glands ( glands of Krause and glands of wolfring )
The mucin glands
- Goblet cells. These are unicellular mucous glands located abundantly within the epithelium of all the regions of the conjunctiva except the marginal mucocutaneous junction and limbal conjunctiva. The goblet cells are formed from the deepest cells( basal layer) of the conjunctiva and migrate towards the surface. These cells are destroyed after discharging their content, the mucin . The density of goblet cells is high in children and young adults. They are more numerous on the nasal side, perticularly in the bulbar conjunctiva and inferior fornix.
The conjunctival-associated lymphoid tissue (CALT) consists of T and B lymphocytes, without plasma cells. Further, lymphoid aggregation corresponding to the mucosal associated lymphoid tissue (MALT) of the gut and bronchi are also found in the conjunctiva.
The Goblet cells are round or oval in shape with an eccentric flattened nucleus near the base of the cell. It contains a prominent Golgi apparatus with numerous mucus pockets in the cytoplasm.
The mucin secreted by goblet cells lubricates and protects the epithelial cells of the conjunctiva and the cornea and ensures the tear film Stability by lowering the surface tension.
The absence of tear fluid has no effect on the dedication, but destruction of the goblet cells as in epithelial xerosis ( hypovitaminosis A ) and parenchymatous xerosis , leads to dessication of the conjunctiva. The number of goblet cells is greatly increased in the inflammatory conditions.
2.Henle’s glands: Crypts of Henle are not true glands but folds of the mucous membrane present in the palpebral conjunctiva between tarsal plates and the fornices . These are tubular structures with lumina of 15-30 micrometre which contains a few goblet cells . These resemble Lieberkuhn’s crypts in the large intestine.
- Glands of Manz: These are found in the limbal conjunctiva in animals like pig, calf or ox. Their existence in human begins is controversial.
These Glands secret mucus which is essential for wetting the cornea and conjunctiva.
The Accessory Lacrimal Glands
These include:
Glands of Krause
Glands of wolfring
Rudimentary accessory lacrimal glands
Glands of Krause: These are microscopic glands lying in the sub-conjunctival tissue of the fornices . These are about 40-42 in the upper fornix and about 6-8 in the lower fornix. Their ducts unite to form a long duct which opens in the fornix.
Glands of wolfring: These are microscopic glands present along the upper border of superior tersus (2-5 in number ) , and lower border of inferior tarsus ( 2-3 in number ).
Rudimentary accessory lacrimal glands: These are present in the caruncle,plica semilunaris and infraorbital region.
Each of these glands has a tubular lumen 15 to 30 μm in diameter that opens onto the conjunctival surface. These glands are formed by an invagination of the conjunctival epithelium and are lined with mucus-secreting epithelial cells.
The nasal tarsal conjunctiva contains numerous structures known as Henle’s mucus crypts. These crypts change in the midtarsal conjunctiva to form a network of subepithelial grooves. The grooves become tunnels with multiple interconnections that have small openings onto the ocular surface. The grooves and tunnels divide the surface of the conjunctiva into irregular papillae averaging approximately 100 μm in diameter . At the orbital margin of the tarsus, the tunnel system opens onto the surface to form a network of grooves that divide the surface into bulges averaging 300 μm in diameter. In the fornix, these grooves and clefts are called Stieda’s cleft and plateau system. These structures are generally larger and more prominent on the temporal side,7 and are usually more prominent in the upper eyelid than in the lower fornix. The patterns made by these clefts and grooves differ greatly between the conjunctivas of different individuals, as well as between the eyes of one individual. Local or systemic disease processes may result in hypertrophy of the underlying lymphoid layer, with follicle formation and profound alterations in the surface features of the conjunctiva. The conjunctival papillae that are normally present may also hypertrophy in response to infectious or toxic agents, and thus further modify the surface topography.