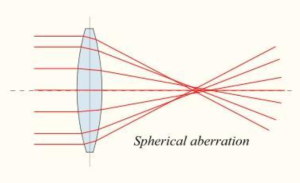
Cornea is a transparent, avascular, aspheric structure of the eye-ball.It is centrally steep and peripherally flat.It consists of 1/6th of the fibrous coat of the eyeball. Some amount of vascularization is present at the peripheral part of the cornea.
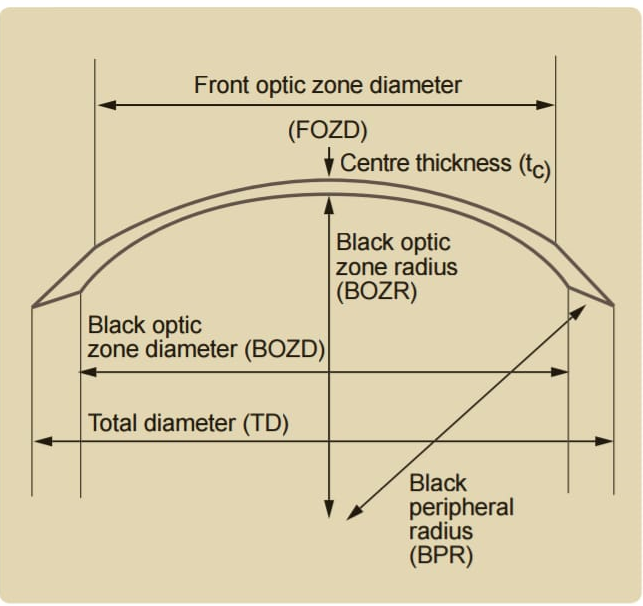
Corneal curvature plays an important role for the refraction.Always it is remembered that above the cornea, tear film plays an important role for refraction during contact lens fitting.
Cornea Is Centrally Thin (0.52mm)compared to periphery (0.67mm). Central portion of the cornea (5 mm) is responsible for the refractive zone. Anterior radius of curvature is 7.8 mm and posterior radius of curvature is 6.5 mm.
For The Refraction,cornea is responsible for 3rd/4th of the eyeball.
It Means:
C=(60*3/4)=45.00 D.
Refractive index of corneais 1.37.
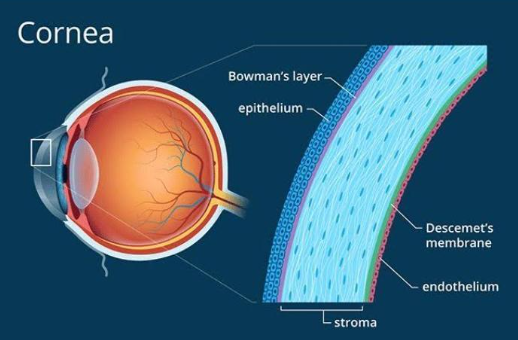
Layers Of Cornea:
1.Epithelium
2.Bowman’s membrane
3.Stroma
4.Descemet’s membrane
- Endothelium
1.Epithelium:
It is the super most layer of the cornea.It is a regenerative layer.
Epithelium is about 50 to 60 µm thick and it consist of three layers:
- Squamous cell layer.
- Wing cell layer.
- Basal cell layer.
2.Bowman’s membrane:
It consists of a cellular mass. If it is damaged then it does not regenerate. It shows considerable resistance from injury.
3.Stroma:
It is the thickest layer of the cornea. It is usually 0.5mm thick. It
consists of collagen fibrils and it consist of 200 -300 layers.
4.Descemet’s membrane:
It is a homogenous layer and bound to stroma posteriorly. Its thickness increases with age. It is made up of collagen and glyco-protein, no elastic materials are present. It is strongly resistance to trauma, foreign body etc. It can regenerate after damage.
5.Endothelium:
It consists of single cell layer .Each cell is Hexagonal in shape. As age increases the number of cells decreases. These cells once damaged will not regenerate.
Some diseases and disorders of the cornea are:
Allergies- Allergies affecting the eye are fairly common. The most common allergies are those related to pollen, particularly when the weather is warm and dry. Symptoms can include redness, itching, tearing, burning, stinging, and watery discharge, although they are not usually severe enough to require medical attention. Antihistamine decongestant eye drops can effectively reduce these symptoms, as does rain and cooler weather, which decreases the amount of pollen in the air.
An increasing number of eye allergy cases are related to medications and contact lens wear. Also, animal hair and certain cosmetics, such as mascara, face creams, and eyebrow pencil, can cause allergies that affect the eye. Touching or rubbing eyes after handling nail polish, soaps, or chemicals may cause an allergic reaction. Some people have sensitivity to lip gloss and eye makeup. Allergy symptoms are temporary and can eliminated by not having contact with the offending cosmetic or detergent.
Conjunctivitis (Pink Eye) –This term describes a group of diseases that cause swelling, itching, burning, and redness of the conjunctiva, the protective membrane that lines the eyelids and covers exposed areas of the sclera,or white of the eye.Conjunctivitis can spread from one person to another and affects millions of Americans at any given time. Conjunctivitis can be caused by a bacterial or viral infection, allergy, environmental irritants, a contact lens product, eye drops, or eye ointments.
At its onset, conjunctivitis is usually painless and does not adversely affect vision. The infection will clear in most cases without requiring medical care. But for some forms of conjunctivitis, treatment will be needed. If treatment is delayed, the infection may worsen and cause corneal inflammation and a loss of vision.
Corneal Inflection – Sometimes the cornea is damaged after a foreign object has penetrated the tissue, such as from a poke in the eye. At other times, bacteria or fungi from a contaminated contact lens can pass into the cornea. Situations like these can cause painful inflammation and corneal infections called keratitis. These infections can reduce visual clarity, produce corneal discharges, and perhaps erode the cornea. Corneal infections can also lead to corneal scarring,which can impair vision and may require a corneal transplant.
As a general rule, the deeper the corneal infection, the more severe the symptoms and complications. It should be noted that corneal infections, although relatively infrequent, are the most serious complication of contact lens wear.
Minor corneal infections are commonly treated with anti-bacterial eye drops. If the problem is severe, it may require more intensive antibiotic or anti-fungal treatment to eliminate the infection,as well as steroid eye drops to reduce inflammation. Frequent visits to an eye care professional may be necessary for several months to eliminate the problem.
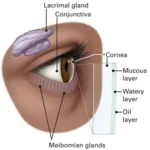
Dry Eye- The continuous production and drainage of tears is important to the eye’s health. Tears keep the eye moist, help wounds heal, and protect against eye infection. In people with dry eye, the eye produces fewer or less quality tears and is unable to keep its surface lubricated and comfortable.
The tear film consists of three layers – an outer, oily (lipid) layer that keeps tears from evaporating too quickly and helps tears remain on the eye; a middle (aqueous) layer that nourishes the cornea and conjunctiva; and a bottom(mucin) layer that helps to spread the aqueous layer across the eye to ensure that the eye remains wet. As we age, the eyes usually produce fewer tears. Also, in some cases, the lipid and mucin layers produced by the eye are of such poor quality that tears cannot remain in the eye long enough to keep the eye sufficiently lubricated.
The main symptom of dry eye is usually a scratchy or sandy feeling as if something is in the eye. Other symptoms may include stinging or burning of the eye; episodes of excess tearing that follow periods of very dry sensation; a stringy discharge from the eye; and pain and redness of the eye. Sometimes people with dry eye experience heaviness of the eyelids or blurred, changing, or decreased vision, although loss of vision is uncommon.
Dry eye is more common in women, especially after menopause. Surprisingly, some people with dry eye may have tears that run down their cheeks. This is because the eye may be producing less of the lipid and mucin layers of the tear film, which help keep tears in the eye. When this happens, tears do not stay in the eye long enough to thoroughly moisten it.
Dry eye can occur in climates with dry air, as well as with the use of some drugs, including antihistamines, nasal decongestants, tranquilizers, and anti-depressant drugs. People with dry eye should let their health care providers know all the medications they are taking, since some of them may intensify dry eye symptoms.
People with connective tissue diseases, such as rheumatoid arthritis, can also develop dry eye. It is important to note that dry eye is sometimes a symptom of Sjögren’s syndrome, a disease that attacks the body’s lubricating glands, such as the tear and salivary glands. A complete physical examination may diagnose any underlying diseases.
Artificial tears, which lubricate the eye, are the principal treatment for dry eye. They are available over-the-counter as eye drops. Sterile ointments are sometimes used at night to help prevent the eye from drying. Using humidifiers, wearing wrap-around glasses when outside, and avoiding outside windy and dry conditions may bring relief. For people with severe cases of dry eye, temporary or permanent closure of the tear drain (small openings at the inner corner of the eyelids where tears drain from the eye) may be helpful.
Fuchs’ Dystrophy – Fuchs’ dystrophy is a slowly progressing disease that usually affects both eyes and is slightly more common in women than in men. Although doctors can of ten see early signs of Fuchs’ dystrophy in people in their 30s and 40s, the disease rarely affects vision until people reach their 50s and 60s.
Fuchs’ dystrophy occurs when endothelial cells gradually deteriorate without any apparent reason. As more endothelial cells are lost over the years, the endothelium becomes less efficient at pumping water out of the stroma. This causes the cornea to swell and distort vision. Eventually, the epithelium also takes on water, resulting in pain and severe visual impairment.
Epithelial swelling damages vision by changing the cornea’s normal curvature, and causing a sight- impairing haze to appear in the tissue. Epithelial swelling will also produce tiny blisters on the corneal surface. When these blisters burst, they are extremely painful.
At first, a person with Fuchs’ dystrophy will awaken with blurred vision that will gradually clear daring the day .This occurs because the cornea is normally thicker in the morning.
it retains fluids during sleep that evaporate in the tear film while we are awake. As the disease worsens, this swelling will remain constant and reduce vision throughout the day.
When treating the disease, doctors will try first to reduce the swelling with drops, ointments, or soft contact lenses. They also may instruct a person to use a hair dryer, held at arm’s length or directed across the face, to dry out the epithelial blisters. This can be done two or three times a day.
When the disease interferes with daily activities, a person may need to consider having a corneal transplant to restore sight. The short-term success rate of corneal transplantation is quite good for people with Fuchs’ dystrophy. However, some studies suggest that the long-term survival of the new cornea can be a problem.
Herpes Zoster (Shingles) : This infection is produced by the varicella-zoster virus, the same virus that causes chickenpox. After an initial outbreak of chickenpox (often during childhood), the virus remains inactive within the nerve cells of the central nervous system. But in some people, the varicella-zoster virus will reactivate at another time in their lives. When this occurs, the virus travels down long nerve fibers and infects some part of the body, producing a blistering rash (shingles), fever, painful inflammations of the affected nerve fibers, and a general feeling of sluggishness.
Varicella-zoster virus may travel to the head and neck, perhaps involving an eye, part of the nose, cheek, and forehead. In about 40 percent of those with shingles in these areas, the virus infects the cornea. Doctors will often prescribe oral anti-viral treatment to reduce the risk of the virus infecting cells deep within the tissue, which could inflame and scar the cornea. The disease may also cause decreased corneal sensitivity, meaning that foreign matter, such as eyelashes, in the eye are not felt as keenly. For many, this decreased sensitivity will be permanent.
Although shingles can occur in anyone exposed to the varicella-zoster virus, research has established two general risk factors for the disease: (1) Advanced age; and (2) A weakened immune system.
Pterygium: A pterygium is a pinkish, triangular-shaped tissue growth on the cornea. Some pterygia grow slowly throughout a person’s life, while others stop growing after a certain point. A pterygium rarely grows so large that it begins to cover the pupil of the eye.
Pterygia are more common in sunny climates and in the 20-40 age group. Scientists do not know what causes pterygia to develop. However, since people who have pterygia usually have spent a significant time outdoors, many doctors believe ultraviolet (UV) light from the sun may be a factor. In areas where sunlight is strong, wearing protective eyeglasses, sunglasses, and/or hats with brims are suggested. While some studies report a higher prevalence of pterygia in men than in women,this may reflect different rates of exposure to UV light.
Because a pterygium is visible, many people want to have it removed for cosmetic reasons. It is usually not too noticeable unless it becomes red and swollen from dust or air pollutants. Surgery to remove a pterygium is not recommended unless it affects vision. If a pterygium is surgically removed, it may grow back, particularly if the patient is less than 40 years of age. Lubricants can reduce the redness and provide relief from the chronic irritation.