Introduction
Symblepharon is a severe ocular condition in which the conjunctiva adheres to the inner surface of the eyelid. The adhesion may cause discomfort, reduce the vision and in serious cases loss of ocular mobility. The prognosis of symblepharon is essential to know in order to understand the early diagnosis and treatment.
Causes of Symblepharon
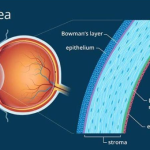
Severe or long-lasting inflammation of your conjunctiva can lead to symblepharon. Your conjunctiva lines the insides of your eyelids and the white part of your eyeball. Severe inflammation and swelling can make these tissues stick together. Scarring follows, making the adhesions permanent.
Sometimes, your cornea may also be inflamed (keratoconjunctivitis). That’s the clear membrane that covers your iris. This can lead to adhesions between your conjunctiva and cornea. Conditions that can cause severe conjunctivitis or keratoconjunctivitis include infections, injuries and autoimmune disease.
Some examples include:
– Ocular herpes
– Trachoma
– Adenoviral keratoconjunctivitis
– Chemical burns
– Complications of eye surgery
– Adverse reaction to eye medications
– Graft vs. Host disease
– Ocular cicatricial pemphigoid
– Mucous membrane pemphigoid
– Bullous pemphigoid
– Erythema multiforme
– Stevens- johnson syndrome
– Lichen planus
– Scleroderma
– Sarcoidosis
– Granulomatosis with polyangitis
Symptoms of Symblepharon
The symptoms of symblepharon can vary depending on the severity of adhesion. Some common symptoms include:
-Eye discomfort and irritation
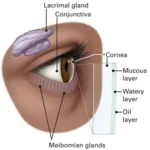
-Dryness and foreign body sensation
-Limited eye movement
-Blurred vision due to corneal involvement
-Redness and inflammation
-Difficulty in blinking
Prognosis of Symblepharon
The prognosis of symblepharon largely depends on the underlying cause, early intervention, and the effectiveness of treatment. Without timely management, the condition can worsen,
leading to-
Chronic discomfort: Persistent irritation and dryness due to conjunctival scarring.
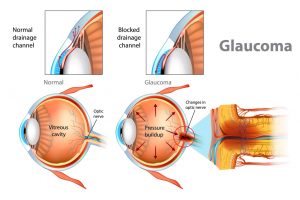
Corneal damage: Adhesions can extend to the cornea, affecting vision and increasing the risk of blindness.
Severe visual impairment: In extreme cases, symblepharon can cause vision loss, especially when associated with autoimmune disorders.
Recurrence: Even after treatment, the condition may recur if the underlying cause remains unresolved.
Diagnosis and Tests
Your eye care provider can diagnose symblepharon with an eye exam. They can give you eye drops to make it more comfortable. During your exam, they’ll carefully observe which tissues are attached, and where. They’ll also look for complications that can occur with the type of symblepharon you have.
If they don’t already know what’s causing your symblepharon, your provider might suggest additional tests to find out, like an eye swab or a blood test. Some of the possible causes will go away with treatment, but others are chronic conditions that may continue to occur and need ongoing treatment.
Treatment and Management
Symblepharon treatment aims to restore eye function and prevent further complications. Options include:
Lubricating Eye Drops and Ointments: These help in reducing discomfort and dryness.
Anti-inflammatory Medications: Corticosteroids or immunosuppressive drugs can be used to control inflammation.
Surgical Intervention: In severe cases, surgical procedures such as mucous membrane
grafting or amniotic membrane transplantation may be required.
Artificial Eye Shells: These can be used to prevent adhesions in early stages.
Treatment of Underlying Conditions: Managing autoimmune diseases or infections is crucial
in preventing recurrence.
Symblepharon surgery
If your provider can’t prevent symblepharon or they’re treating you after the fact, you may need
surgery to remove the adhesions. Surgery for symblepharon varies depending on how severe it
is. You may only need a simple procedure, or you may need complex oculoplastic surgery. Methods may include:
– Symblepharon release: This simply means disconnecting the adhesions between your
conjunctiva layers. Your surgeon might also need to remove scar tissue from your conjunctiva.
– Tissue graft: Surgeons may use tissue from elsewhere on your eyeball or from another
mucous membrane like the inside of your lip, to replace tissue they remove from your eye.
– Oculoplastic reconstruction: If your symblepharon affected your conjunctiva fornix, your
surgeon might need to reconstruct it. If it affected your cornea, you might need keratoplasty.
Complication-
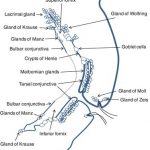
Symblepharon can irritate your eye by interfering with blinking or by turning your eyelashes in
toward your eye (trichiasis). A symblepharon that involves your conjunctiva fornix may obstruct
your tear system. A symblepharon that restricts your eye movement, or that attaches to your
cornea, can cause vision loss.
Conclusion
Symblepharon is a potentially debilitating eye condition that requires prompt diagnosis and
intervention. While mild cases can be managed with lubrication and medication, severe cases
may necessitate surgical correction. The prognosis largely depends on early detection and the
effective management of underlying conditions. Regular eye check-ups and proper eye care are
essential in preventing the progression of this condition and ensuring better visual outcomes.