WHAT IS RETINOSCOPY?
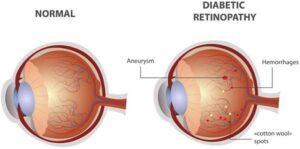
Retinoscopy is a technique to objectively determine the refractive error of the eye. (farsighted, nearsighted, astigmatism) and the need for glasses. The test can be quick, easy, reliably accurate and requires minimal cooperation from the patient.
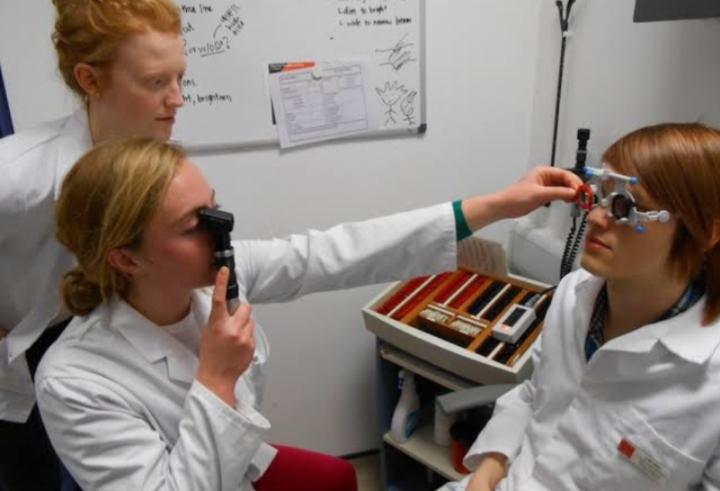
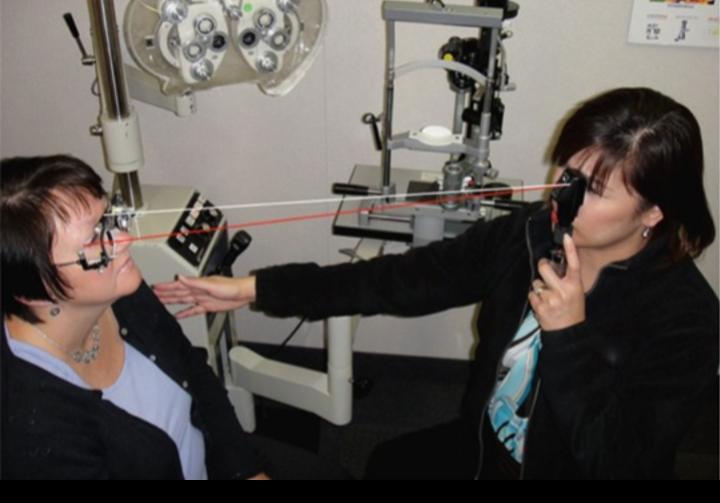
HOW IS IT PERFORMED?
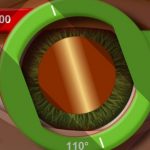
A handheld instrument called a retinoscope projects a beam of light into the eye. When the light is moved vertically and horizontally across the eye, the examiner observes the movement of the reflected light from the back of the eye. This reflection is called the red reflex. The examiner then introduces lenses in front of the eye and as the power of the lenses changes, there is a corresponding change in the direction and pattern of the reflection. The examiner keeps changing the lenses until reaching a lens power that indicates the refractive error of the patient.
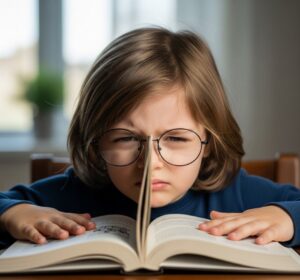
Retinoscopy is particularly useful in prescribing corrective lenses for patients who are unable to undergo a subjective refraction that requires a judgement and response from the patient (such as children or those with severe intellectual disabilities or communication problems). In most tests however, it is used as a basis for further refinement by subjective refraction. It is also used to evaluate accommodative ability of the eye and detect latent hyperopia.
DARK ROOM TEST
Retinoscopy should preferably be conducted in a dark room.
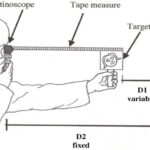
1) Examiner sits at 1meter away from the patient. It is even more convenient to sit at arm’s length, i.e two- third meter away , so that lenses can be held in the other hand while the light beam is passed. The point of reversal is then 1.5D
The patient is normally seated and looking towards the far end of the room (relaxed eye)
Sources of light from behind the patient.
The optometrist looks through a plane mirror with central perforation, and light is reflected in to the patient’s eye.
The mirror is slowly moved from side to side in different meridians, and movement of the shadow is noted.
There are two types of retinoscopy Static and dyanamic.
Static retinoscopy is performed when the patient has relaxed accommodative status. This can be obtained by the patient viewing a distance target or by the use of cycloplegic drugs (where, for example, a child’s lack of reliable fixation of the target can lead to fluctuations in accommodation and thus the results obtained). Dynamic retinoscopy is performed when the patient has active accommodation from viewing a near target.
WHEN IS RETINOSCOPY USED?
Retinoscopy is used to determine refractive error in children, developmentally delayed adults, or in individuals whose behavior limits the ability to be cooperative with other refraction techniques. It is especially useful in very young children and infants.
There are dry and wet retinoscopy. Dry’ retinoscopy refers to various techniques that can be performed to determine the refractive state of the eye without the use of pharmacological agents such as cycloplegics…. When such agents are used the technique is referred to as ‘wet’ retinoscopy.
ARE DILATING EYE DROPS NECESSARY FOR RETINOSCOPY?
Children’s eyes are typically dilated for retinoscopy. This is because the reflex is easier to see when the pupil is large and because the drops temporarily limit the eye’s ability to accommodate or focus. This allows for a more accurate determination of the refractive error.
PROCEDURE
(CYCLOPLEGICS)
It is required in children’s and Young patients. In adults and old patient’s it is usually not necessary.
1) If the patient is less than 5 years: Atropine eye ointment (1%) is to be applied three times daily for 3 days.
2) If the patient is between 5 and 15 years: (1%) cyclopentolate ,or (2%) homatropine eye drops is instilled for 3 times, about 1 hour before examination.
3) If the patient is between 15 and 20 years:
The same procedure is under taken.
The refraction under cycloplegia is always pathological because the shape of the lens has been altered. A post cycloplegic test(PCT) is therefore advisable.