Introduction
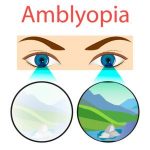
Screening children’s vision at a young age is
recommended to detect signs of potential
disorders such as amblyopia, strabismus and
refractive error, which can affect the child’s
visual development. Early treatment of reduced
vision is particularly important in children as
treatment is age-sensitive and should be
started as early as possible.
Take detailed history
As with every patient encounter, whether with
adults or children, it is critically important to
have a detailed understanding of the patient’s
symptoms, medical history, and family history
to help and guide. This information will also
help to tailor and target the clinical
examination. Ask the parents about recent
changes in behavior. Pictures and videos of the
child may be helpful. Family history can also
provide important clues about the patient’s
condition.
Engage parents and patients
It is very important to build a rapport with the patient
and the family. Try to keep everyone relaxed and put the
child at ease. This will take some time, but it will
potentially increase the level of cooperation by the child.
Engaging the child with games, multicolor flashing lights,
toys, and high-fives, showing cartoons on video
monitors, or providing positive reinforcement with
stickers may help distract or relax the patient.
Increasingly, parents have smartphones or tablets
preloaded with the patient’s favorite videos and songs,
and these can be helpful distractions.
Excellent communication with explanation of every step
of the examination is critical in gaining both the patient’s
and parents’ trust. Cooperative parents can help children
feel more secure and play a key role in assisting with the
examination. Pretending to examine one of the parents
first occasionally helps to reassure the patient. With very
young infants, having the parents or an assistant hold the
patient down may be required, but this should not
necessarily be the first step for all examinations.
Male the exam engaging
In the examination proper, try to pique the patient’s
interest in the proceedings. For example, ask the child
whether he or she can see the examiner’s eyes from the
other end of the instrument, or tell the patient that the
examiner is going to try to find a dinosaur or other object
of interest in the eye. Another useful trick is to ask the
child what color he or she thinks the examination light is.
For early school-age children, having the patient stand up
at the slit lamp may sometimes be preferred
ergonomically over sitting down for the examination.
Objective testing techniques:
Objective testing techniques play a critical role in
assessing the vision of non-verbal children. These tests
do not rely on the child’s verbal feedback but provide
direct visual function measurements. Some standard
objective tests include:
Retinoscopy: This technique involves shining a light
into the child’s eyes and observing the reflected light
from the retina. The optometrist can estimate the
child’s prescription by analyzing how the light moves
in response to the eye’s refractive error.
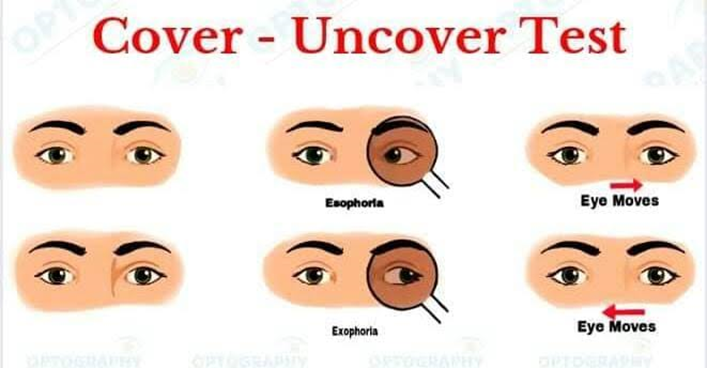
Fixation Behavior: Optometrists observe the child’s
ability to fixate on and follow objects. The inability to
maintain steady eye fixation may indicate eye
movement disorders or other visual problems.
Pupil Reflex Testing: Pupil reflexes are assessed by
shining a light into the eyes and observing the pupil’s
response. This test can help identify neurological
issues or optic nerve abnormalities.
Teller Acuity Cards: These cards contain patterns
that decrease in size, and the optometrist observes
the child’s responses to determine visual acuity
levels.
Subjective refraction:
When children are older (commonly 6 to 7 years or
above) and can respond to instructions, subjective
refraction can be performed. The subjective refraction
should begin with maximum plus for hyperopic children
and least minus for myopic children and reach the
subjective endpoint using 0.25D increments or
decrements. Since undercorrection is not useful in
managing myopia, it is important to provide the
refractive error that provides the best vision. A
duochrome test can be performed monocularly or
binocularly to check on the best vision sphere. While
performing the duochrome test, if the letters/rings on
the green side of the chart appear darker/clearer,
increase by +0.25D steps and decrease by -0.25D steps if
the letters/rings on the red side of the chart appear
darker/clearer. The child needs to tell the clinician which
side of the chart the letters appear “darker/clearer.” The
endpoint of the test is when letters on both the red and
green side of the chart appear equally dark/clear to the
patient. Finally, a Jackson’s cross-cylinder technique can
be used to fine-tune the cylinder power and axis for
older children.
Summary
Although it is challenging to perform refractive error
assessments in young children but it is rewarding when a
successful outcome is achieved and the child and their
parents are satisfied with the outcome. Because children
adapt and learn rapidly, practitioners will find it easier to
perform refraction at follow-up visits.