Glaucoma is not a single disease process but a group of disorders characterized by a progressive optic neuropathy resulting in a characteristic appearance of the optic disc and a specific pattern of irreversible visual field defects that are associated frequently but not invariably with raised intraocular pressure (IOP). Thus, IOP is the most common risk factor but not the only risk factor for development of glaucoma. Consequently, the term ‘ocular hypertension’ is used for cases having constantly raised IOP without any associated glaucomatous damage. Conversely, the term normal or low tension glaucoma is semuggested for the typical cupping of the disc and /or visual field defects associated with a normal low IOP.
DEFINITION:-Glaucoma is a symptomatic condition where the functional integrity of the eye is disturbed, resulting in characteristics irreversible loss of visual field due to persistent raised IOP.
CLASSIFICATION OF GLAUCOMA:-
i) CONGENITAL OR DEVELOPMENTAL:
a) PRIMARY- Due to primary developmental anomaly at the angle.
b) SECONDARY-Associated with ocular or systemic disorders.
ii) ACQUIRED:
a) PRIMARY ANGLE-CLOSURE GLAUCOMA (PACG) -Is characterized by apposition of peripheral iris against the trabecular meshwork(TM) resulting in obstruction of aquous outflow by closure of an already narrow angle of the anterior chamber. The condition is not associated with any other ocular and systemic abnormalities.
b) PRIMARY OPEN ANGLE GLAUCOMA (POAG) -As the name implies, it is a type of primary glaucoma, where there is no obvious systemic or ocular cause of rise in the intraocular pressure. Primary open-angle glaucoma (POAG), also known as chronic simple glaucoma of adult onset is typically characterised by:
•Slowly progressive raised intraocular pressure.
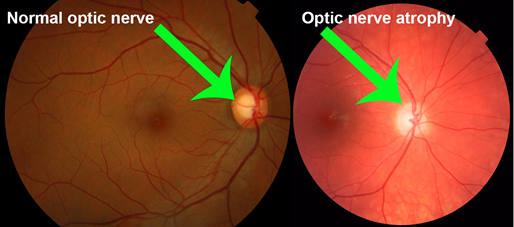
•Characteristic optic disc cupping
•Specific visual field defects.
c) SECONDARY GLAUCOMA-Secondary is not a disease entity but a group of disorders in which rise of intraocular pressure is associated with some primary ocular or systemic disease.
classification-
A) Depending upon the rise in IOP
B) Depending upon the causative primary disease secondary glaucomas are named as follows.
1) lens-induced(phacogenie) glaucomas.
2) Inflammatory glaucoma (Glaucoma due to intraocular inflammation)
3) Pigmentary glaucoma
4) Neovascular glaucoma
5) Glaucoma associated with iridocorneal endothelial syndrome
6) Psedoexfoliative glaucoma
7.Glaucomas associated with intraocular hemorrhage
8) Steroid-induced glaucoma
9) Traumatic glaucoma
10) Glaucoma -in-aphakia
11) Glaucoma associated with intraocular tumors.
SYMPTOMS:-
CONGENITAL OR DEVELOPMENTAL-
•Marked photophobia
•Blepharospasm
•watering
PRIMARY ANGLE-CLOSURE GLAUCOMA-
Prodromal stage-
•Colored halos around the light
•Blurring of vision
•Occasional headache
Acute congestive attack-
•Acute, intense, unbearable pain, radiating along the distribution of 5 th cranial nerve.
•Severe headache often with nausea and vomiting, often mistaken for an acute abdomen
•Marked dimness if vision, is mainly due to ischemic optic Neuropathy and party due to corneal edema.
•Redness , lacrimation and photophobia.
PRIMARY OPEN-ANGLE GLAUCOMA-
•Painless , progressive loss of vision
•Mild headache or eye ache
•Incresing difficulty in near worsks and frequent change of presbyopic glasses. This is due to accommodative failure owing to pressure upon the ciliary muscle.
•Delayed dark adaption may develop, a disability which becomes increasing disturbing in the late stages.
•Scotoma may be noticed occasionally by some observant patients.
•significant loss of vision and blindness is the end result of untreated cases of POAG.
SIGNS:-
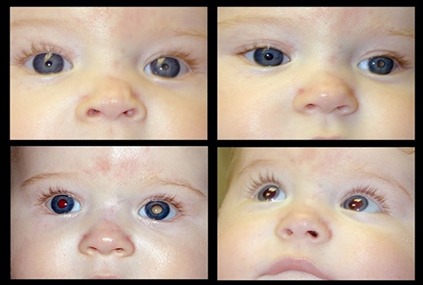
CONGENITAL & DEVELOPMENTAL-
•Eyeball becomes enlarged, if the IOP becomes elevated prior to age of 3 years. This enlarged eyeball due to glaucoma, is known as bupthalmos.
•cornea is enlarged, globular and steamy. Corneal sensation is diminished.
•Anterior chamber deep.
•Tremulousness of the iris with patches of atrophy.
•Lens is flattened and displayed backward. There may be subluxation.
•The patient becomes myopic. But the amount of myopia is less than anticipated from the increased axial length.
PRIMARY ANGLE-CLOSURE GLAUCOMA-
•Eyeball:Tenderness present.
•Eyelids:Marked edema with narrowing of the palpebral aperture.
•Conjunctiva:Both ciliary and conjuntival congestion with chemosis.
•cornea is steamy and insensitive.
•Anterior chamber vety shallow. Cells and flare may be present.
•Iris pattern is lost and discolored.
•IOP:Markedly elevated
•Fundus cannot be visualized due to haze cornea. But after instillation of glycerin drop the fundus may be visible.
•The fellow eye, usually has a shallow anterior chamber and a narrow angle.
PRIMARY OPEN-ANGLE GLAUCOMA-
•Visual acuity may remain good till the late stage.
•cornea is usually clear.
•Anterior chamber depth is normal.
•pupillary reaction remains normal until the last stage.
•Increased IOP with a large diurnal variation.
•Cupping of the optic disc.
•Raised IOP
•Classical visual field defects.
SECONDARY GLAUCOMA-
There are many types of glaucoma. Common types are:-
•Psedoexfoliative glaucoma:characteristic white exfoliative material is seen on the anterior lens capsule in three distinct concentric zone.
•Phacomorphic glaucoma:A swollen intumescent cataract may cause secondary angle-closure glaucoma.
•Phacolytic glaucoma:A secondary open-angle glaucoma due to microleak of lens capsule in a hyper mature or rarely in a mature cataract.
•Neovascular glaucoma: Secondary glaucoma is associated with neovascularization of the iris and angle of the anterior chamber. It’s classically seen in-
i) Diabetic retinopathy
ii) Central retinal venous occlusion (CRVO)
iii) Sickle cell retinopathy
iv) Caroticocavernous fistula
•Traumatic glaucoma:A blunt injury to the eye may cause secondary glaucoma by several mechanism. In many cases, more than ine mechanism is involved ,they are:
i) Traumatic iridocyclitis
ii) Hyphema
iii) Massive intraocular hemorrhage
iv) Subluxation or dislocation of the lens
v) trabecular damage, etc