Non-strabismic binocular vision disorders (NSBVDs) are subtle but clinically significant anomalies of the vergence and accommodative systems. Unlike strabismus, they do not involve a constant ocular deviation, yet they can cause considerable visual discomfort, reduced efficiency, and impaired academic performance. Accurate diagnosis requires a systematic evaluation of multiple parameters, each compared against established normal ranges. By analyzing these findings in combination, clinicians can classify disorders such as convergence insufficiency, accommodative infacility, fusional vergence dysfunction, and others.
Case History and Symptoms
The diagnostic process begins with a detailed case history. Patients often report eyestrain,
headaches, blurred vision, intermittent diplopia, difficulty concentrating, or reduced reading
fluency. These symptoms typically worsen with prolonged near work and may improve with rest.
Importantly, NSBVDs are functional disorders, so subjective complaints must be correlated with
objective test results.
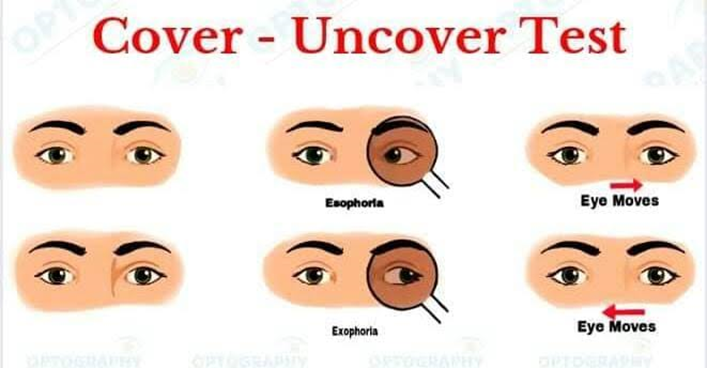
Cover Test and Phoria Assessment
The cover test is the foundation of binocular vision evaluation. It reveals latent deviations (phorias) at both distance and near.
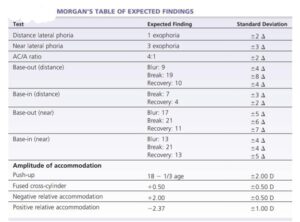
Normal ranges: Distance phoria is typically 0–2Δ exophoria, while near phoria is 0–6Δ exophoria.
Diagnostic use: Exophoria at near beyond 6Δ suggests convergence insufficiency (CI), while esophoria at near beyond normal indicates convergence excess (CE). Large deviations at distance point toward divergence disorders. Equal phoria at distance and near, within normal ranges, is consistent with basic phorias.
AC/A Ratio
The accommodative convergence to accommodation (AC/A) ratio quantifies the relationship between accommodation and convergence.
Normal range: 3–5:1.
Diagnostic use: A low AC/A ratio (<3:1) is typical of CI and divergence insufficiency, reflecting inadequate convergence for a given accommodative demand. A high AC/A ratio (>5:1) is seen in CE and divergence excess, reflecting excessive convergence linked to accommodation. A normal AC/A ratio is associated with basic exophoria, basic esophoria, and fusional vergence dysfunction (FVD).
Near Point of Convergence (NPC)
NPC measures the closest point at which the eyes can maintain fusion.
Normal range: Break ≤6 cm, recovery ≤10 cm.
Diagnostic use: A receded NPC (>6–7 cm) is a hallmark of CI. A normal NPC is
observed in accommodative disorders and basic phorias. NPC testing is particularly sensitive in detecting CI, often correlating strongly with patient-reported symptoms of near fatigue and diplopia.
Vergence Amplitudes
Vergence ranges, assessed with prism bars or phoropters, evaluate the ability to maintain fusion under stress.
Normal ranges: At near, base-out (BO) ranges should be 15–20Δ, and base-in (BI) ranges 10–15Δ.
Diagnostic use: Reduced BO ranges indicate CI, reduced BI ranges suggest CE or divergence excess, and reduction in both BO and BI ranges is diagnostic of FVD.
Stereopsis
Stereopsis testing assesses depth perception.
Normal range: ≤40 arc seconds on standard tests.
Diagnostic use: Reduced stereopsis (>60 arc sec) is common in CI, CE, and FVD, reflecting compromised binocular integration. Normal stereopsis is typically preserved in accommodative disorders.
Accommodative Facility
Accommodative facility testing, performed with ±2.00 D flippers, evaluates the speed and flexibility of accommodation.
Normal range: 11–13 cycles per minute (cpm) monocularly.
Diagnostic use: Difficulty with +2.00 D lenses indicates accommodative insufficiency, difficulty with –2.00 D lenses suggests accommodative excess, and difficulty with both lenses is diagnostic of accommodative infacility.
Binocular Accommodative Facility
Binocular facility testing requires simultaneous coordination of accommodation and vergence.
Normal range: 8–10 cpm.
Diagnostic use: Patients with CI or CE often fail binocular facility despite normal monocular performance. Accommodative infacility manifests as failure under both monocular and binocular conditions.
Relative Accommodation (NRA/PRA)
NRA and PRA measure the ability to relax and stimulate accommodation while maintaining fusion.
Normal ranges: NRA is +2.00 ± 0.50 D, PRA is –2.37 ± 0.50 D.
Diagnostic use: Low PRA is characteristic of accommodative insufficiency, low NRA indicates accommodative excess, and both reduced values suggest accommodative infacility or ill-sustained accommodation.
MEM Retinoscopy
MEM retinoscopy assesses accommodative lag or lead.
Normal range: +0.25 to +0.75 D lag of accommodation.
Diagnostic use: A high lag (>+0.75 D) supports a diagnosis of accommodative insufficiency, while a lead of accommodation (against motion reflex) indicates accommodative excess.
Ocular Motor Function
Ocular motor testing evaluates saccades and pursuits.
Normal range: Age-appropriate, accurate, and sustained movements without fatigue or loss of fixation.
Diagnostic use: Deficits indicate ocular motor dysfunction, a separate category in the classification system.
Diagnostic Profiles
By synthesizing these parameters, clinicians can classify NSBVDs into distinct categories:
Convergence Insufficiency: Exophoria at near beyond 6Δ, low AC/A, NPC >6 cm, BO
<15Δ, reduced stereopsis, normal monocular facility but poor binocular, low PRA, normal MEM.
Convergence Excess: Esophoria at near beyond 6Δ, high AC/A, normal NPC, BI <10Δ, reduced stereopsis, poor binocular facility, low NRA, normal MEM.
Fusional Vergence Dysfunction: Normal phoria, normal AC/A, normal NPC, both BO and BI reduced, reduced stereopsis, normal monocular facility but poor binocular, normal NRA/PRA, normal MEM.
Accommodative Insufficiency: Normal phoria, normal AC/A, normal NPC, normal ranges, fails +2.00 monocular, binocular poor, low PRA, high lag on MEM.
Accommodative Excess: Normal phoria, normal AC/A, normal NPC, fails –2.00 monocular, binocular poor, low NRA, accommodative lead on MEM.
Accommodative Infacility: Normal phoria, normal AC/A, normal NPC, fails both +2.00 and –2.00 monocular, poor binocular, low NRA and PRA, normal MEM.
Divergence Insufficiency: Esophoria at distance, low AC/A, normal NPC, reduced BI ranges, reduced stereopsis, normal accommodative facility, poor binocular facility, low NRA, normal MEM.
Divergence Excess: Exophoria at distance, high AC/A, normal NPC, reduced BO ranges, reduced stereopsis, normal accommodative facility, poor binocular facility, low PRA, normal MEM.
Basic Exophoria/Esophoria: Equal phoria at distance and near, normal AC/A, normal NPC, normal ranges, normal stereopsis, binocular facility poor, NRA/PRA normal, MEM normal.

Conclusion
The diagnosis of NSBVDs relies on recognizing consistent patterns across multiple parameters
rather than isolated findings. Each test—cover test, AC/A ratio, NPC, vergence ranges,
stereopsis, accommodative facility, NRA/PRA, and MEM—provides a piece of the puzzle.
When combined, they form a diagnostic profile that allows clinicians to classify the disorder
accurately and tailor management strategies accordingly. This parameter-based approach ensures
precision, enhances patient outcomes, and provides a robust framework for both clinical practice
and academic teaching.
Reference:
[1] Scheiman, Mitchell(2014), Clinical management of binocular vision