The Goldmann applanation tonometer (GAT) is considered accurate, highly reliable, and simple to use. Moreover, this instrument is extremely well established in clinical use and research.
In 1948, Hans Goldmann proposed GAT to measure IOP.To this date, GAT remains the gold standard method for measuring IOP and is most
frequently used by ophthalmologists in a routine clinical setting. It utilizes applanation, which measures the force required to compress the
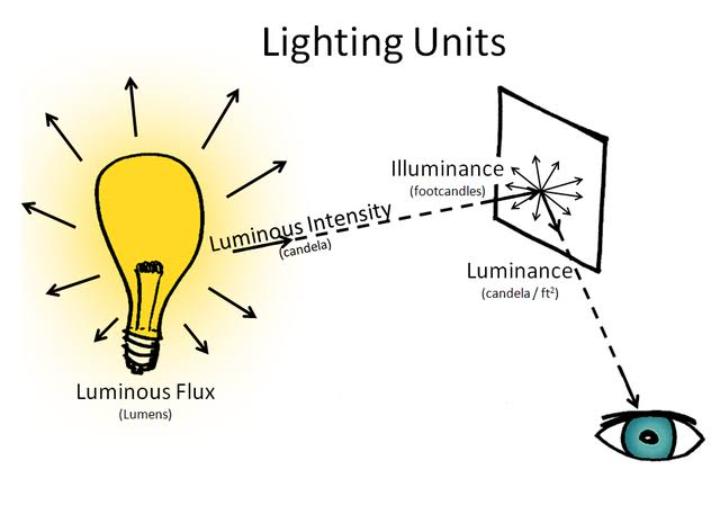
cornea over a given area. Applanation tonometry is based on the Imbert- Fick law from the 1800s, which states that the pressure inside the eye (P)
can be approximated by the force (F) needed to flatten a fixed area of the cornea divided by the surface area (S) of the flattened region of the surface. The higher the intraocular pressure, the greater the force needed to compress the cornea.
Goldmann Applanation Tonometry
Principle
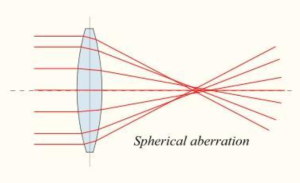
Goldmann applanation tonometer is based on the Imbert–Fick principle, which states that for a dry thin-walled sphere, the pressure (P) inside the
sphere equals the force (F) necessary to flatten its surface divided by the area (A) of flattening (i.e. P = F/A). It applies to surfaces which are
perfectly spherical, dry, flexible, elastic and infinitely thin. Theoretically, average corneal rigidity (taken as 520 μm for GAT) and the capillary
attraction of the tear meniscus cancel each other out when the flattenedarea has the 3.06 mm diameter contact surface of the Goldmann prism,
which is applied to the cornea using the Goldmann tonometer with ameasurable amount of force from which the IOP is deduced.
The effects of corneal rigidity and tear film surface tension forces approximately cancel when the area applanated is 7.35 mm2. When applanating this area, a force of 0.1 g corresponds to an IOP of 1 mmHg.
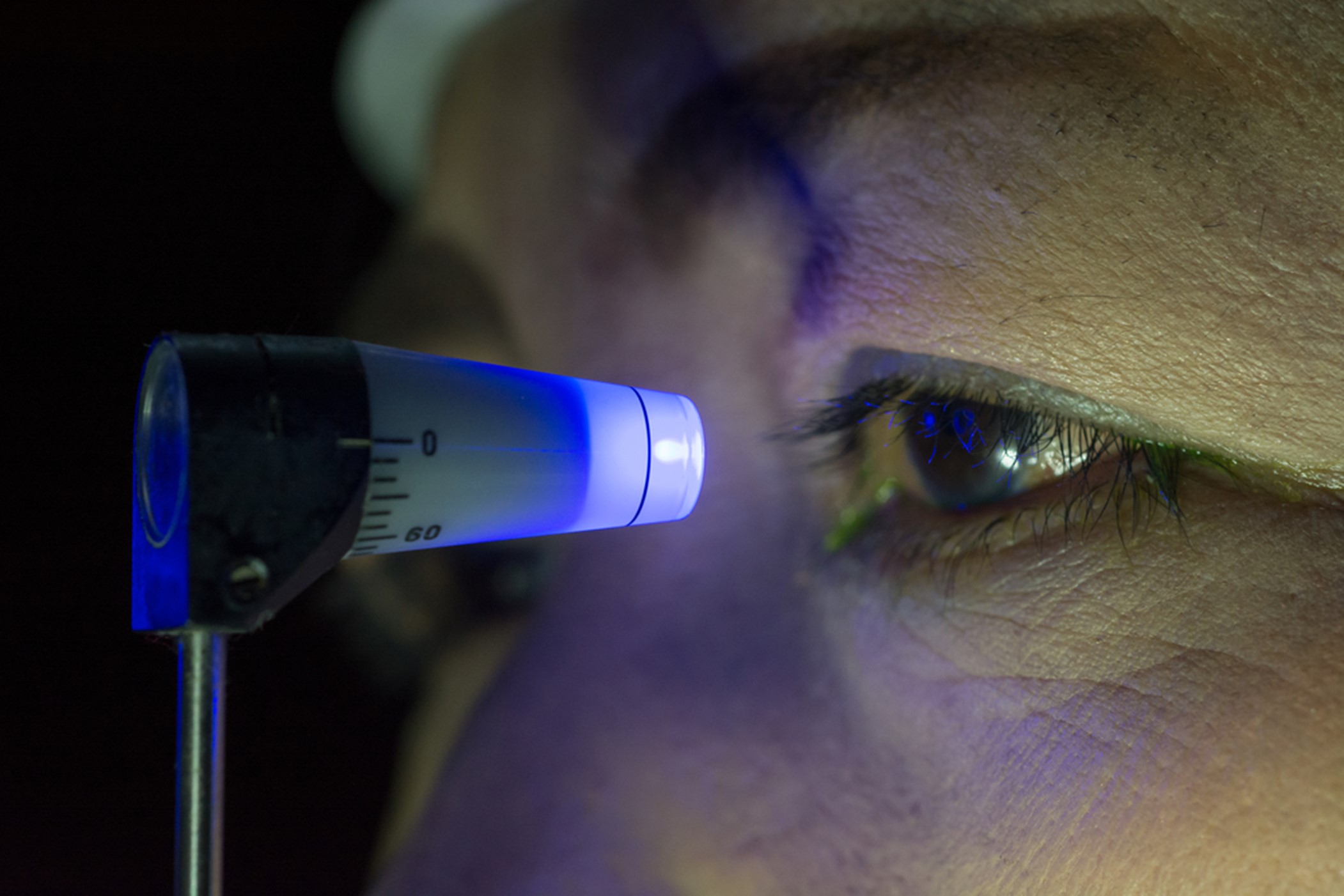
GAT is the reference standard for tonometry. The GAT is slit-lamp mounted and is available in a modified hand-held form (the Perkins tonometer). When viewed through the slit lamp, the tonometer biprism splits the image of the fluorescent tear meniscus into two semicircular rings. A dial on the side of the tonometer is adjusted to vary the force applied to the eye, causing a movement of the rings either together or apart. The end point is achieved when the inner edges of the semicircles touch .
Goldmann Applanation Tonometry procedure
Patient set up:
1. Explain procedure to patient: It is important the patient fully understands what you are going to do, including the (minimal) risks
involved.
2. Check for allergies.
3. Make sure that the patient doesn’t have any tight clothing around the neck.
4. Ask the patient to remove any hats. Look for anything else that may obstruct the tonometer e.g. Dermatocalasis, unkempt eye brows, facial hair etc.
5. Adjust the patient’s chair and slit lamp height.
6. Instil chosen anaesthetic and fluorescein combination – make sure you tell the patient it stings and it’s yellow!
7. Note drops used, time used and their expiry on the record card.
8. Ask the patient to place their chin on the chin rest; forehead against the bar. Remind them to keep still, keep their teeth together, and try not to hold their breath.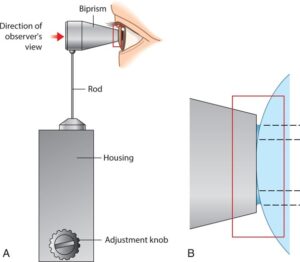
Slit lamp set up:
1. Place the probe in the probe holder. Make sure you support
the neck while you do this.
2. For traditional probes, line up the zeros. For Tonosafe,
ensure the flat edge is at the top.
3. Set the dial to the 15mmHg mark.
4. Place the tonometer on the guide plate. It can go in either circular slot to start with. You only need to swap the slot if you feel the probe is at the wrong angle to catch the corneal apex. The guide plate should be placed with the tapered end towards the patient.
5. Clean chin rest and forehead bar in front of patient.
6. Set magnification to x10.
7. Adjust illumination to maximum.
8. Flip to the cobalt blue filter.
9. Set illumination system to 45°. Put on your right side for the patient’s left eye. Put on your left side for the patient’s right eye.
Goldmann procedure:
1. Ask the patient to fixate a distant object.
2. Hold the upper lid against the patient’s brow. Try to make sure you are not touching the globe. If the patient has a wide palpebral aperture you may get away with not holding the lids.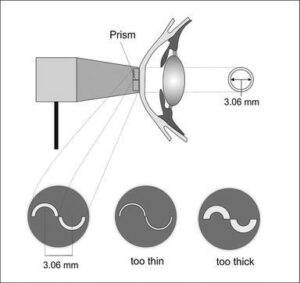
3. Come close to the eye and briefly touch the cornea. Make sure you are ‘just’ touching the corneal apex. As soon as the mires appear you should stop nudging the tonometer forward.
4. Adjust the dial on the side of the tonometer to position the mires so that their inner edges are touching. Read off the number on the dial, multiplying by 10 to get the reading in mmHg.
5. Note IOP measurement including the time the IOP was taken.
The GAT has some limitations, including:
It requires local anesthetics
It can be difficult for patients with poor compliance, surgical patients, and children
It’s nonportable
It requires sterilization
It needs to be calibrated