Explain About IOL Power Calculation
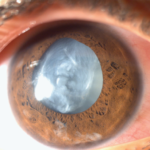
Intraocular lens (IOL) power calculation is a crucial process in cataract surgery to determine the appropriate power of the artificial lens that will replace the eye’s natural lens. The goal is to achieve the desired refractive outcome, ideally providing the patient with optimal vision without the need for corrective eyewear. This process involves several steps and relies on precise measurements and sophisticated formulas.
Here’s a detailed overview of the process: Key Components of IOL Power Calculation:
• Preoperative Measurements:
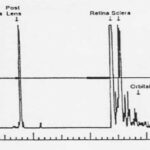
Biometry (Axial Length measurement) : The distance from the front of the cornea to the retina. It is typically measured using ultrasound or optical coherence biometry (e.g., IOLMaster Anterion or Lenstar devices).
Keratometry (K-values): Measurements of the corneal curvature. These values help determine the refractive power of the cornea.
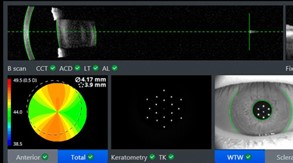
Anterior Chamber Depth (ACD): The distance between the corneal endothelium and the anterior lens capsule. This is important for accurately placing the IOL.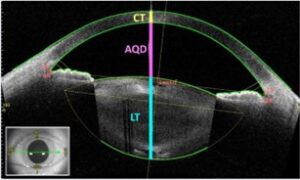
Lens Thickness (LT): The thickness of the natural lens, which can also influence the final IOL power calculation.
Lens Constants: These are specific to the type of IOL being used and are critical for accurate calculations. They include parameters like A-constant, SRK/T constant, and Haigis constants, which are provided by the IOL manufacturer.
• IOL Power Calculation Formulas
Different generations of formulas have been developed to improve the accuracy of the calculations and the ability to predict the effective lens position. For example, the SRK-T, Hoffer-Q, Holladay-2, and Haigis formulas have been used to calculate IOL power.
1. First-Generation Formulas:
• SRK (Sanders-Retzlaff-Kraff): An early formula that laid the groundwork for later developments.
2. Second-Generation Formulas:
• SRK II: An improved version of the SRK formula incorporating a correction factor based on the axial length of the eye.
3. Third-Generation Formulas:
• SRK/T: Combines the original SRK formula with theoretical considerations.
• Holladay: Incorporates more detailed biometric data and a regression analysis.
• Hoffer Q: Particularly effective for shorter eyes.
• Haigis: Utilizes three constants to fine-tune the calculation, incorporating modern measuring devices.
4. Fourth-Generation Formulas:
• Barrett Universal II: Uses a universal approach applicable to a wide range of eye types, often considered one of the most accurate.
• Hill-RBF: An artificial intelligence-based formula that utilizes a large database of patient outcomes.
• Olsen: Incorporates precise measurements of the eye’s internal structures and an advanced algorithm.
• Effective Lens Position (ELP):
ELP is an estimation of where the IOL will sit within the eye post-surgery. It significantly affects the refractive outcome and is estimated based on preoperative measurements.
• Personalization and Optimization:
Modern IOL power calculation often involves personalization, where the chosen formula is adjusted based on the surgeon’s own outcomes and patient population. Postoperative refractive outcomes are used to refine future calculations, making them more precise.
• Special Considerations:
Eyes with prior refractive surgery: Traditional formulas might not work as well for patients who have had LASIK or PRK. Specialized formulas or adjustments (e.g., the Haigis-L formula) are used in these cases.
High axial myopia or hyperopia: Special consideration and sometimes different formulas are used for eyes with very short or very long axial lengths.
Toric IOLs: For patients with significant astigmatism, toric IOLs can be implanted. Calculating the power and axis for these lenses requires additional steps and considerations.

Biometry Technology: Advanced optical biometers (e.g., IOLMaster 700, Lenstar) provide highly accurate measurements and often incorporate the latest IOL power calculation formulas.
• Advances and Technology:
Swept-Source OCT and other advanced biometry devices: These provide highly accurate measurements and can integrate with IOL calculation software for improved outcomes.
Artificial Intelligence (AI) and Machine Learning: These are being integrated into IOL power calculation to analyze vast amounts of data and improve prediction accuracy.
• Practical Application
Gather Data: Perform thorough measurements of the eye’s axial length, corneal curvature, and anterior chamber depth using reliable instruments.
Select Formula: Choose an appropriate calculation formula based on the eye’s characteristics and the type of IOL being implanted.
Input Data: Enter the measurements into the selected formula along with the
lens constants provided by the IOL manufacturer.
Review Output: The formula will provide the recommended IOL power. Review the results, considering the patient’s visual needs and any specific conditions (e.g., post-refractive surgery adjustments).
Verification and Adjustment: Double-check calculations, especially in complex cases, and make any necessary adjustments based on clinical judgment. By carefully following these steps, surgeons can significantly improve the accuracy of IOL power calculations, leading to better visual outcomes for patients undergoing cataract or refractive lens surgery. In summary, IOL power calculation is a sophisticated and evolving field that combines precise measurements with advanced mathematical models to ensure optimal visual outcomes for cataract surgery patients.