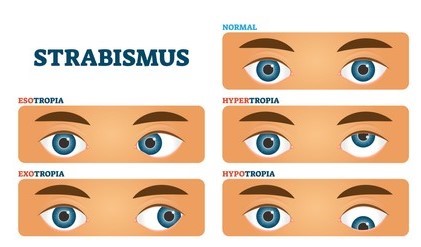
Introduction: Concomitant esotropia is the inward deviation of one eye. It is the most common type of squint in children. It can be unilateral or alternative.
Clinico-etiological types of Concomitant esotropia:
1. Infantile esotropia 2. Accommodative esotropia 3. Acquired non-accommodative esotropia 4. Sensory esotropia 5. Consecutive esotropia
1. Infantile esotropia
Age: 2-4 months, may occur in the first 6 months of life.
The angle of deviation- is constant and fairly large.
Fixation pattern- BSV does not develop, alternative fixation in primary gaze, cross fixation in lateral gaze.
Amblyopia- In 25 to 45% of cases.
Association–
।. Inferior oblique over action.
।।. Dissociated vertical deviation. (DVD)
।।।. latent horizontal nystagmus.
Treatment
1. amblyopia treatment – eye patching
2. recession both medial rectus. It is preferred over the unilateral Recess Recet procedure.
3. time of surgery – 6 months to 2 years. preferably before 1 year.
2. Accommodative Esotropia
Definition- It is defined as the inward deviation of one eye caused by accommodation convergence associated with hyperopia. It is the most common type of strabismus in children.
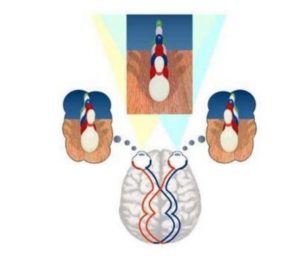
Etiology- Hyperopia accommodative convergence, esotropia.
Risk Factor- Hyperopia [> + 2.00 D], Family history, illness of Teoma pathology- age – between 2-4 years, sex and race – no predilection, moderate hyperoxia
Types –
1. Refractive accommodative esotropia
2. non-refractive accommodative esotropia
3. mix accommodative esotropia
Refractive accommodative esotropia – Normal AC/A ratio, 2-3 years with moderate hyperoxia, for both near and distance, can be corrected with spectacle.
Non-refractive accommodative esotropia – large AC/A ratio, may occur with non-refractive error, its occur near> distance, may correct with bifocal glass.
Mix accommodative esotropia –
High AC/A ratio, combination hypermetropia, it occurs due to near>= distance, may correct with bifocal or spectacle.
Diagnosis- 1. cover uncover test 2. worth four dot test 3. after-image test 4. Synaptophoreclinical features — Patients will complain of eyes crossing only when the child is tired or focusing on something close.
Symptoms- 1. Diplopia 2. The blurring of vision management — general treatment with spectacle correction ( cycloplegia surgery – recommended only when >10prisamD fresnel prism can be tried before surgery. surgical option — Bilateral medial rectus recetion Monocular rece – recet procedure.
Complication – 1. amblyopia 2. diplopia 3. derotation of esotropia
3. Acquired non-accommodative esotropia: this amount of deviation is not affected by accommodation, it includes essential acquired esotropia 1. basic. 2. convergence 3. divergence in suffence
Treatment –
1. Surgery 2. Acquired concomitant esotropia 3. Nystagmus 4. Esotropia in myopia and microtropia
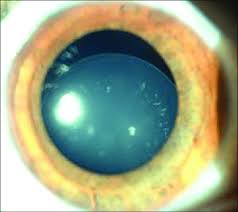
4. Sensory esotropia – Result from non-ocular lesions. Such as – Cataracts, Ptosis, Aphakia, Anisometropia, Optic atrophy, and Retinoblastoma 5. Consecuative esotropia — Result for surgical over carrection of exotropia.
**Test for concomitant esotropia —
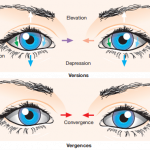
1. Cover Test — * direct cover test – It confirms the presence of manifest squint. To perform it, the patient is asked to fixate on a point light. Then, the normal-looking eye is covered while observing the movement of the uncovered eye. In the presence of squint, the uncovered eye will move in the opposite direction to take fixation, while in apparent squint there will be no movement. This test should be performed for near texation ( at 33 cm) and distance texation( at 6 meters).
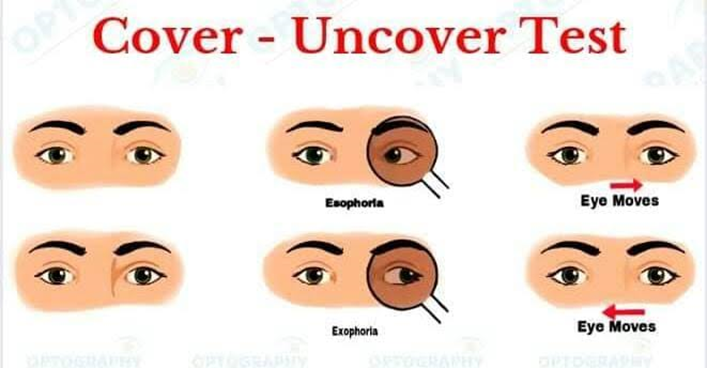
* Cover uncovers test – It tells about the presence and type of heterophoria. To perform it, one eye is covered with an occluder and the other is made to fix an object. In the presence of heterophoria, the eye undercover will deviate. After a few seconds, the cover is quickly removed and the movement of the eye (which was undercover) is observed. The direction of movement of the eyeball tells the type of heterophoria (e.g., the eye will move outward in the presence of esophoria)and the speed of movement tells whether recovery is slow or rapid.
* Alternative cover test- It reveals whether the squint is unilateral or alternate and also differentiates concomitant squint from paralytic squint (where the secondary deviation is greater than primary).
2. Prism cover test- Prisms of increasing strength with the apex towards the deviation are placed in front of one eye and the patient is asked to fixate an object with the other. The cover-uncover test is performed till there is no recovery movement of the eye undercover. This will tell the amount of deviation in prism dioptres. Both heterophoria, as well as heterotopia, can be measured by this test.
3. Hirschberg corneal reflex test – It is a rough but handy method to estimate the angle of manifest squint. In it, the patient is asked to fixate at point light held at a distance of 33 cm and the deviation of the corneal light reflex from the center of the pupil is noted in the squinting eye. Roughly, the angle of squint is 15o and 45o when the corneal light reflex falls on the border of the pupil and limbus, respectively.
4. Modified krimsky corneal reflex test – In this test the patient is asked to fixate on a point light and prisms of increasing power (with the apex towards the direction of a manifest squint) are placed in front of the normal fixating eye till the corneal light reflex is centered in the squinting eye. The power of prism required to center the light reflex in the squinting eye equals the amount of squint in prism dioptres.
5. Worth four dot test
6. Test for fixation
7. After the image test
8. Natural density filter test
9. Synoptophore
Treatment–
1. Spectacles with full correction of refractive error.
2. Occlusion therapy- Done below 10 years – Normal eye is occluded after correcting the refractive error. And the patient is advised to use the squinting eye.
3. Preoperative orthoptic exercises- Done after correction of amblyopia to overcome suppression.
4. Squint surgery – Done after correction of refractive error amblyopia and orthoptic exercises.
Basic principles of squint surgery
1. Recession- shifting the insertion of muscles posteriorly .- to weaken the strong muscles
2. Resection- shorting the muscles.- to strong than the weak muscles.
3. Post-operative orthoptic exercises- to improve fusion and BSV.