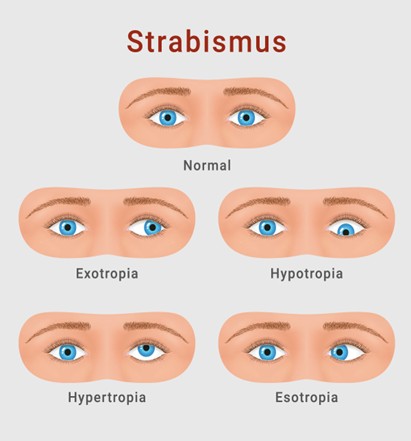
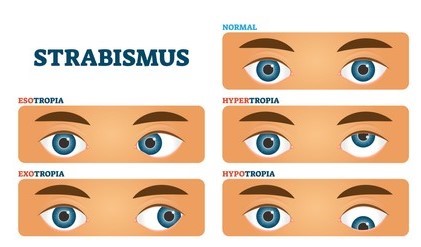
Strabismus, commonly referred to as a “squint,” is a misalignment of the eyes in which the visual axes fail to maintain parallelism. One eye may deviate inward (esotropia), outward (exotropia), upward (hypertropia), or downward (hypotropia), while the fellow eye maintains fixation. Strabismus is among the most frequently encountered ocular disorders in pediatrics, with a prevalence of approximately 2–4%.
Although often perceived as a cosmetic concern, untreated strabismus may result in suppression, amblyopia, defective binocular vision, and impaired stereopsis. Early diagnosis and timely intervention are therefore essential to ensure optimal visual development in children.
Diagnosis of Strabismus in Children
The diagnosis of strabismus requires a detailed clinical evaluation, incorporating history- taking, visual assessment, ocular alignment tests, and ancillary investigations.
1. History
• Age of onset of deviation.
• Frequency (constant vs intermittent).
• Associated symptoms (diplopia)
• Family history of strabismus or refractive errors.
• Perinatal and systemic history (neurological conditions, developmental delay).
2. Visual Acuity Assessmentt
Depending on the child’s age, visual acuity may be tested using:
• Preferential looking tests (Teller acuity cards, Cardiff cards).
• Lea symbols or picture charts.
• Snellen’s or LogMAR charts for cooperative older children.
3. Ocular Alignment Tests
• Corneal Light Reflex Test (Hirschberg Test): Assesses approximate deviation by observing the position of the corneal light reflex.
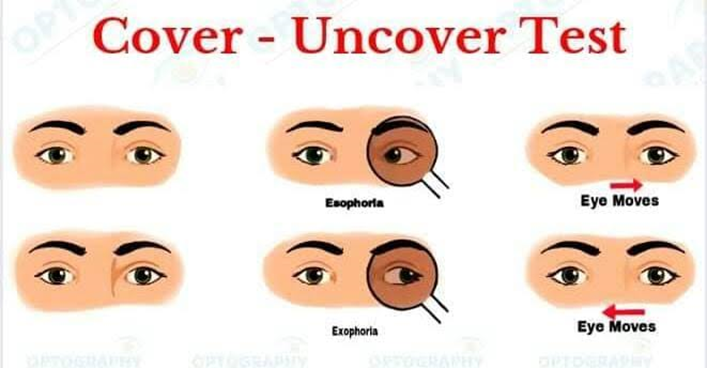
• Cover–Uncover Test: Identifies manifest deviations (tropias).
• Alternate Cover Test: Quantifies total deviation (latent + manifest).
• Prism Bar Cover Test (PBCT): Measures the angle of deviation in prism diopters.
4. Ocular Motility Examination
Evaluation of ductions and versions to detect any restrictive or paralytic strabismus.
5. Cycloplegic Refraction
Performed after instillation of cycloplegic drops (commonly cyclopentolate or atropine) to assess refractive error accurately, as uncorrected hypermetropia is a common cause of accommodative esotropia.
6. Binocular Vision and Stereopsis Tests
• Worth 4-dot test.
• Synoptophore evaluation.
• Random dot stereograms.
7. Fundus Examination
To rule out sensory strabismus secondary to ocular pathology (e.g., cataract, macular scar, optic nerve hypoplasia).
Treatment Options for Strabismus
The primary goals of treatment are:
• To preserve or restore visual acuity.
• To achieve ocular alignment.
• To promote binocular single vision and stereopsis.
1. Optical Correction
• Spectacles: Full hypermetropic correction is prescribed in accommodative esotropia.
• Bifocals: Indicated in high accommodative convergence/accommodation (AC/A) ratio.
2. Amblyopia Management
• Occlusion Therapy: Patching of the dominant eye to stimulate the amblyopic eye.
• Pharmacological Penalization: Atropine drops in the better-seeing eye as an
alternative to patching.
3. Orthoptic and Vision Therapy
Includes convergence exercises and fusion training, particularly useful in intermittent exotropia and convergence insufficiency.
5. Surgical Intervention
Indicated when conservative measures fail or in cases of large, constant deviations.
• Recession (weakening procedure) or resection (strengthening procedure) of extraocular muscles.
• Surgery is often performed bilaterally in symmetrical deviations.
• Timing is crucial: early surgery (within 6–24 months of onset) may optimize binocular potential.
Prognosis and Importance of Early Intervention Children have a sensitive period of visual development, typically up to 7–8 years of age.
Intervening during this period offers the best chance of achieving normal binocular function. Delayed treatment may result in irreversible amblyopia, loss of stereopsis, and psychosocial challenges.
Conclusion
Strabismus in children is a condition that requires prompt recognition, precise diagnosis, and individualized management. With advances in optical correction, amblyopia therapy, orthoptic training, botulinum toxin, and surgical techniques, most children can attain good visual outcomes and improved quality of life. A comprehensive pediatric eye examination is indispensable whenever ocular misalignment is suspected. Early referral and timely treatment can make the difference between a lifetime of visual disability and the gift of clear, coordinated vision.