Introduction –
Retinal detachment is one of the most serious vision-threatening conditions encountered in eye care practice. As optometrists, we often see patients who initially present with subtle visual complaints, not realizing that these symptoms may indicate a retinal emergency. Unfortunately, delayed presentation remains a major reason for poor visual outcomes. Understanding the warning signs of retinal detachment and acting promptly can make the difference between saving vision and permanent vision loss.
Understanding Retinal Detachment –
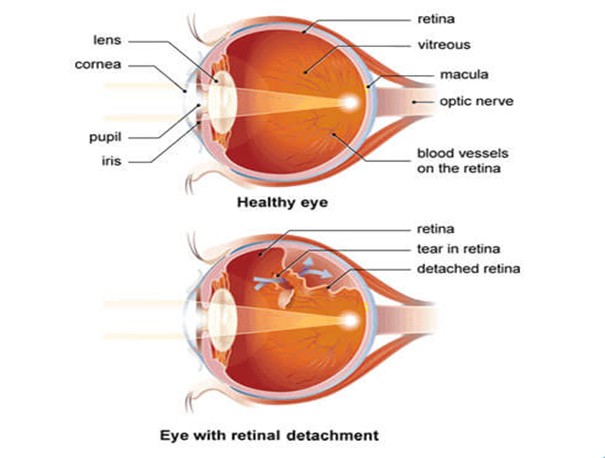
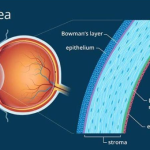
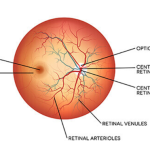
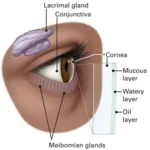
The retina is a thin, delicate, light-sensitive layer of neural tissue lining the inner surface of the eye. It plays a critical role in vision by converting light into electrical signals that are transmitted to the brain via the optic nerve. For the retina to function properly, it must remain attached to the underlying retinal pigment epithelium and choroid, which provide oxygen and essential nutrients.
Retinal detachment occurs when the retina separates from these supporting layers. Once detached, the retinal tissue becomes metabolically compromised. If reattachment is delayed, irreversible damage to photoreceptor cells can occur, leading to permanent vision loss.
One of the most dangerous aspects of retinal detachment is that it is usually painless, which often leads patients to underestimate the seriousness of their symptoms.
Why Retinal Detachment Is an Ocular Emergency:
From a clinical standpoint, retinal detachment is a true ocular emergency. Visual
prognosis depends largely on:
– How quickly the condition is diagnosed
– Whether the macula (central retina) is involved
– The duration of retinal separation
If the macula is still attached at the time of treatment, visual outcomes are generally
much better. Once the macula detaches, even successful surgery may not fully restore
central vision. This is why early symptom recognition and immediate referral are
essential.
Early Warning Symptoms Patients Should Never Ignore:
Doctor & Optometrists consistently emphasize that sudden changes in vision are never
normal. The following symptoms should prompt immediate eye examination, preferably with pupil dilation.
1. Sudden Flashes of Light (Photopsia)
Patients may complain of seeing brief flashes or flickers of light, often in peripheral vision or in dim lighting conditions. These flashes are commonly caused by vitreoretinal traction, where the vitreous gel pulls on the retina. This traction can lead to a retinal tear, which may progress to retinal detachment. New-onset flashes, especially when accompanied by other symptoms, should always be evaluated urgently.
2. Sudden Increase in Floaters
Floaters appear as small black dots, threads, rings, or cobweb-like shadows moving across the field of vision. While occasional floaters are common with aging, a sudden shower of floaters is concerning.
Clinically, this may indicate:
– Posterior vitreous detachment with retinal traction
– Retinal tear
– Vitreous or retinal hemorrhage
Patients often ignore floaters, assuming they are harmless. As optometrists, we must educate patients that a sudden increase in floaters is a red-flag symptom.
3. Shadow, Curtain, or Veil Over Vision
This is one of the most classic and alarming symptoms of retinal detachment. Patients may describe a dark shadow, curtain, or veil moving across their vision from one direction. This usually indicates that a portion of the retina has already detached. At this stage, vision loss may progress rapidly. Immediate referral to a retinal specialist
is critical.
4. Blurred or Distorted Central Vision
When the macula becomes involved, patients may notice sudden blurring, distortion of straight lines, or difficulty reading. Objects may appear smaller, larger, or warped. From a prognostic perspective, macular involvement significantly affects visual recovery. Early detection before macular detachment offers the best chance of preserving
detailed central vision.
5. Loss of Peripheral Vision
Peripheral vision loss may occur gradually and can be easily overlooked by patients. They may bump into objects or feel that their visual field is narrowing.
Careful history-
taking often reveals this symptom in progressing cases of retinal detachment.
Patients at Higher Risk-
Although retinal detachment can occur in any individual, certain patients are at
increased risk and should be monitored more closely:
– High myopia (especially high minus power)
– History of ocular trauma
– Previous intraocular surgery, particularly cataract surgery
– Family history of retinal detachment
– Diabetic retinopathy or other retinal disorders
– Advancing age with vitreous degeneration
Patient education is particularly important for these groups, as early symptom recognition can prevent severe vision loss.
Common Types and Causes of Retinal Detachment:
The most common form is rhegmatogenous retinal detachment, caused by a retinal tear or hole that allows fluid to enter beneath the retina. Tractional retinal detachment is often associated with advanced diabetic eye disease,
where fibrous tissue pulls the retina away. Exudative retinal detachment occurs due to inflammation, tumors, or vascular
abnormalities without a retinal break. Understanding the underlying mechanism helps guide appropriate referral and
management.
Role of the Optometrist:
Optometrists are often the first eye care professionals patients consult when
experiencing visual disturbances. Our role is critical in:
– Identifying early warning signs
– Performing thorough dilated retinal examinations
– Educating patients about symptom urgency
– Making timely referrals to ophthalmologists or retinal specialists
Routine patient counseling, especially for high-risk individuals, is a vital preventive strategy in optometric practice.
Conclusion:
Retinal detachment is a serious but treatable condition when diagnosed early. Unfortunately, many cases present late due to lack of awareness or symptom neglect. As optometrists, emphasizing patient education and early intervention remains one of
our most important responsibilities. Patients should understand that flashes, floaters, shadows, or sudden vision changes are not normal and should never be ignored. Prompt evaluation and referral can preserve vision and significantly improve long-term outcomes. When it comes to retinal detachment, time is vision—and early action truly saves sight.