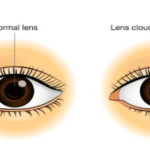
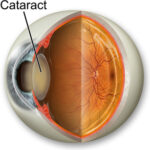
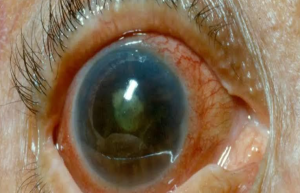
Cataract is also known as waterfall, it defined as any opacity in the lens or its capsule known as cataract which can lead to partial or complete loss of vision. Normally cataract is associated with age , but sometimes it can also occur in congenitally or acquired during childhood. Pediatric cataract represents a significant cause of childhood blindness worldwide. Timely intervention and treatment are necessary to prevent blindness.
Types of cataract :- It based on age onset and morphology.
Congenital cataract: In this cataract seen in birth time.
Developmental cataract: After birth during childhood in this cataract seen.
Traumatic cataract: In this cataract seen after trauma , it can be seen after birth or childhood.
Secondary cataract: This type of cataract associated with systemic or ocular diseases.
Lamellar (zonular) cataract: Most common seen cataract. Opacity involving specific lamellae of the lens.
Nuclear cataract: It involves the central nucleus of the lens.
Polar cataract: It involves the anterior or posterior pole of the lens.
Total cataract: It effects the entire lens .
Cerulean cataract: Small bluish-white opacities scattered throughout the lens.
Coronary cataract: Club-shaped opacities in the cortex. It resembling acrown.
Sutural cataract: Opacity involve the Y-sutures of the lens.
Etiology of Pediatric Cataract
Genetic Causes :- Autosomal dominant inheritance is common, particularly in bilateral congenital cataract. Mutations in genes encoding crystallin proteins.
Intrauterine Infections :- Toxoplasmosis, syphilis, varicella, Rubella, Cytomegalovirus , Herpes simplex virus . Rubella is a classical cause
of congenital cataract , it can be usually bilateral.
Metabolic Disorders :-
Galactosemia: Galactosemia is an autosomal recessive inherited
metabolic disorder. It is caused by a deficiency of the enzyme
galactose. It is caused of oil droplet cataract . It can be
overcome if treated early.
Lowe syndrome: Cataract associated with renal and neurological anomalies.
Hypoglycemia: Hypoglycemia can lead to lens opacities.
Wilson's disease: Rarely causes sunflower cataract.
Systemic Syndromes:- Down syndrome ,marfan syndrome, trisomy 13 and 18
Traumatic Causes :- Blunt or penetrating trauma may lead to unilateral cataract.
Other Causes :- Radiation exposure ,drug-induced such as steroids can increase the risk of cataract.
Clinical Features :-
History:-
Leukocoria – Parental concern regarding white reflex of the lens known as leukocoria.
Nystagmus – Involuntary rapid , jerky movement of the eye . It can lead to poor vision.
Strabismus – Misalignment of the one eyes of both eyes.
Developmental delay associated with symptoms.
Examination:-
Visual acuity: Age-appropriate testing such as fixation pattern, preferential looking, or chart-based methods.
Red reflex: Red reflex can be absent or diminished in affected eyes.
Slit-lamp exam: Can detect types of cataract.
Laterality :-
Unilateral cataracts :- it can be due to idiopathic or traumatic.
Bilateral cataracts: More likely due to genetic, metabolic, orinfectious causes.
Investigations:-
Ocular examination : Slit-lamp biomicroscopy, fundus examination, Intraocular pressure measurement ,Biometry for intraocular lens
power calculation.
Systemic Investigations :-
TORCH titres :- TORCH titres test if intrauterineinfection suspected.
Blood sugar and galactose levels meaure if metabolic cataract suspected.
Urine reducing substances measure for galactosemia.
Karyotyping if syndromic features present.
Management of Pediatric Cataract :-
General Principles:- Early surgery is critical to prevent deprivation
amblyopia. The timing depends on the laterality:
Bilateral dense cataracts: Surgery ideally within 6-8 weeks of age.
Unilateral cataracts: Surgery as early as possible, usually within 4-6 weeks.
Surgical Techniques :-
Lens aspiration with or without primary IOL implantation.Preferred for children over 1 year for IOL implantation. In younger infants (<6 months), aphakia is often preferred initially due to growth of the eye.
Posterior capsulotomy and anterior vitrectomy. Routine in children <6 years to prevent posterior capsule opacification (PCO).
Secondary IOL implantation done at a later age in initially aphakic children.
Intraocular Lens (IOL) Considerations:- IOL power calculationconsiders future eye growth (undercorrection is common).Acrylic foldable lenses preferred. Sulcus placement or scleral fixation if capsular support is inadequate.
Postoperative Management :-
Aggressive amblyopia therapy i.e patching the better eye in unilateral cases.
Spectacles or contact lenses if left aphakic.
Regular follow-up for refraction, IOP monitoring, and detection of complications like PCO or glaucoma.
Visual Rehabilitation :-
Aphakic correction: Contact lenses especially in unilateral cases or spectacles for bilateral aphakia.
Patching therapy: Especially vital in unilateral cases to prevent amblyopia.
Low vision aids: When optimal vision is not achieved post- surgery.
Complications :- Posterior capsule opacification is the most common complication after cataract operation. Secondary glaucoma is also seen after cataract operation and other symptoms can be seen such as IOL decentration, inflammation ,retinal detachment .
Prognosis:-
Bilateral cataract: Better prognosis if operated early.
Unilateral cataract: Visual prognosis guarded due to risk of amblyopia.
Associated ocular anomalies (e.g., microphthalmos, aniridia) worsen prognosis.
Preventive Strategies:-
Maternal rubella immunization before pregnancy.
Early neonatal eye screening.
Genetic counseling for families with hereditary cataract.
Prompt treatment of metabolic disorders (e.g., galactosemia).