Introduction
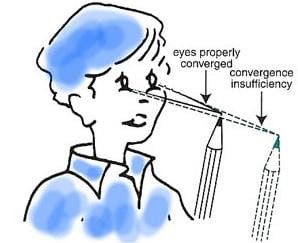
Convergence insufficiency (CI) is one of the most prevalent non-strabismic binocular vision disorders. It affects the ability to maintain proper eye alignment for near tasks, such as reading or using a computer. Characterized by a mismatch between visual demands and the eye’s ability to converge, CI has been reported to affect 3% to 7.7% of the population, with varying prevalence depending on the study
group. This blog delves into the key aspects of convergence insufficiency,
its symptoms, diagnostic criteria, and approaches to management.
Defining Convergence Insufficiency
Convergence insufficiency is primarily diagnosed based on the following:
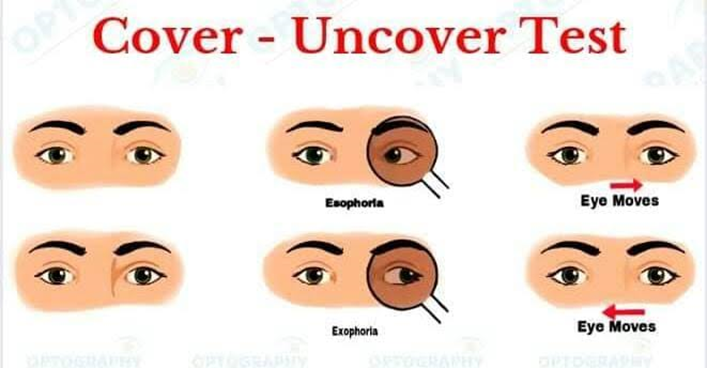
Exophoria at Near: A tendency for the eyes to drift outward while focusing on close objects, greater than the exophoria at distance.
Receded Near Point of Convergence (NPC): Difficulty maintaining convergence for near tasks, leading to a break in fusion.
Reduced Positive Fusional Vergence (PFV): Inability to sustain alignment due to inadequate compensatory convergence.
Low AC/A Ratio: A reduced accommodative convergence to accommodation ratio, often below 3:1. With these primary criteria we are having some secondary criteria like ,
1. Reduced Vergence Facility
2. Reduced Binocular Accomodative Amplitude [ Monocularly good ]
3. Monocular Estimation Method [MEM] shows Lead of Accomodation
Studies by Scheiman et al. and Rouse et al. have provided clarity on the prevalence and diagnostic parameters of CI. These include symptoms and clinical signs, often assessed using standardized tools like the Convergence Insufficiency Symptom Survey (CISS).
Symptoms of Convergence Insufficiency
The symptoms of CI are typically associated with prolonged near work and include:

Eyestrain
Headaches
Blurred or double vision (diplopia)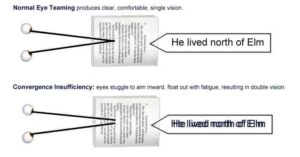
Difficulty concentrating
Loss of comprehension over time
Movement of print or words
Sleepiness during reading or close work
Asymptomatic cases may also occur, often due to suppression or avoidance of
near tasks. Clinicians should inquire about such avoidance behaviors when evaluating for CI. Diagnostic Tools and Criteria
Convergence Insufficiency Symptom Survey (CISS): Standardized questionnaire with 15 items scored from 0 to 4. Scores ≥16 in children (9–17 years) and ≥21 in adults (18+ years) indicate symptomatic CI.
Near Point of Convergence (NPC): Normative values: 5–10 cm for children; 5–7 cm for young adults. Repeated testing may reveal further recession in symptomatic patients.
Positive Fusional Vergence (PFV): Direct and indirect measures indicate the ability to sustain convergence. Reduced vergence facility and difficulty with plus lenses in binocular tests are key
signs.
AC/A Ratio: Typically calculated; values below 3:1 are indicative of CI. Advanced assessments, such as jump convergence tests or the use of red/green glasses during NPC measurements, may add diagnostic sensitivity.
Management and Treatment
The primary goal in managing CI is to alleviate symptoms and improve binocular function. Treatment options include:
Vision Therapy: Evidence-based exercises designed to enhance convergence and improve PFV.
Effective in reducing symptoms as documented in randomized clinical trials.
Prism Correction: Base-in prisms may be prescribed to alleviate near exophoria in select cases.
Home-Based Exercises: Activities like pencil push-ups and computer-based vision therapy can  supplement in-office programs. Regular follow-up is essential to monitor
supplement in-office programs. Regular follow-up is essential to monitor
progress and modify therapy plans.
Research and Future Directions
Ongoing research continues to refine diagnostic protocols and treatment efficacy. The role of neuroplasticity in vision therapy and emerging technologies like virtual reality may revolutionize how we address CI.
Conclusion
Convergence insufficiency is a manageable condition that significantly impacts quality of life, especially for those engaged in prolonged near tasks. Early diagnosis using validated tools like the CISS and targeted interventions such as vision therapy can lead to substantial symptom relief and functional improvement. Optometrists play a crucial role in identifying and managing CI, ensuring patients regain confidence in their visual performance.
References:
[1] Clinical Management of Binocular Vision : Heterophoric , Accomodative , and Eye Movement Disorders [ Fourth Edition ] by Mitchell Scheiman And Bruce Wick
[2] American Academy of Ophthalmology [AAO]