CENTRAL SEROUS CHORIORETINOPATHY (CSCR)
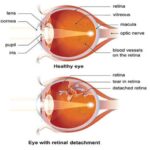
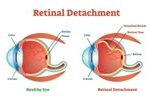
Central serous chorioretinopathy (CSCR) or also known as central serous choroidopathy (CSC) or earlier known as central serous retinopathy (CSR) is characterised by spontaneous serous detachment of neurosensory retina in the macular region, with or without retinal pigment epithelium detachment. The disease was first recognized by Albrecht von Graefe in 1866 and was named central recurrent retinitis. Since then it has been reported under a variety of names such as idiopathic flat detachment of the macula by Walsh et al, central angiospastic retinopathy by Gifford et al, and central serous retinopathy by Straatsma et al. The condition was named Idiopathic central serous chorioretinopathy by Gass et al in 1967.
Etiopathogenesis
Risk factors include:
• Age and sex. The idiopathic disease affects typically young adult (20-50 years), males more than females,
• Personality. Type A personality individuals are more prone,
• Steroid intake is an important risk factor,
• Emotional stress, may also predispose
• Systemic lupus atheromatosis (SLE)
• Pregnancy (usually 3 rd trimester), and • Cushing’s disease are also reported as risk factors.
Pathogenesis is not known exactly. Various theories have been postulated. Presently, the most accepted theory is of ‘choroidal vascular hyperpermeability’. This theory correlates the clinical findings with indocyanine green (ICG) angiography findings. It proposes that sympathetic drive, sympathomimetics and corticosteroids alter the choroidal vascular permeability either directly or indirectly by affecting its autoregulation. This, in turn, increases the tissue hydrostatic pressure in the choroid causing pigment epithelial defect (PED) resulting in a breach in the outer blood retinal barrier. Leakage of fluid across this area results in development of localized serous detachment of neurosensory retina.
Clinical features
Symptoms: patient may present with:
Sudden painless loss of vision (6/9-6/24)
Relative positive scotoma, micropsia & metamorphopsia.
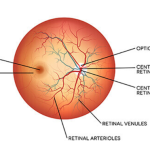
Signs: Biomicroscopic fundus examination reveals:
• Mild elevation of macular area, demarcated by a circular ring reflex.
• Small yellow grey elevations may be seen due to RPE detachment.
• Foveal reflex is absent or distorted (Fig. 12.22).
• Subretinal deposits may be seen.
• Multifocal pigmentary changes suggest chronicity.Clinical course CSCR is usually self-limiting but often recurrent.
Three patterns are known:
Acute classic CSCR is characterized by short clinical course with spontaneous resolution within 3-6 months with near normal visual recovery. Recurrences are known in 30-50% of all the cases. Chronic CSCR, also termed as diffuse retinal pigment epitheliopathy (DRPE), is seen in few cases. It is characterized by a chronic course lasting more than 12 months, typically affecting individuals above 50 years of age. Such cases may have permanent visual impairment due to progressive RPE atrophy and photoreceptor degeneration. Bullous CSCR is rare presentation characterized by = larger and more numerous areas of serous retinal and RPE detachments often confused with bullous retinal detachment. Investigations
1. Fundus fluorescein angiography helps in confirming the diagnosis.
Two patterns of progressive leakage and pooling from one or more points seen are:
• Ink-blot pattern. It consists of small hyperfluorescent spot which gradually increases in size .
•Smoke-stack pattern. It consists of a small hyperfluorescent spot which ascends vertically like a smoke-stack and gradually spreads laterally to take a
mushroom or umbrella configuration.
2. ICG shows multiple areas of hyperfluorescence due to choroidal hyperpermeability.
3. OCT shows neurosensory retinal detachment and accompanying small detachments of the RPE.
Differential diagnosis:
Differential diagnosis of CSR includes other entities which may produce serous detachment of sensory retina in macular area. These include optic pit, idiopathic polypoidal choroidal vasculopathy, macular hole with serous detachment, choroidal tumors and pigment epithelial defect (PED).
Treatment
1.Conservative measures include:Reassurance is the only treatment required in majority of the cases, since CSR undergoes spontaneous resolution in 80 to 90% cases. Visual acuity returns to normal or near normal within 1 to 6 months. Only about 10-20% cases do not have spontaneous resolution. Approximately 20-30% of cases will have one or more recurrences.
Discontinuation of steroids, if possible, should be done at the earliest.
Lifestyle changes to reduces stress in life, should be adopted.
2. Laser photocoagulation is indicated in following Cases:
Long-standing cases (more than 3 months).
•Patients having recurrent CSR with visual loss.
•Patients having permanent loss of vision in the other eye due to this condition. Contraindications Include the cases having leak near or within the FAZ.
3.Photodynamic therapy (PDT) may be beneficial for those with severe disease not amenable to conventional laser treatment, e.g. with sub-
foveal leaks and chronic cases.
4.Anti-VEGF can be considered if CNV develops.
Summary
CSCR is a multifactorial disease without a known mechanism of action. It is most strongly associated with hypercortisolism and is hypothesized to
occur because of choroidal hyperpermeability and secondary RPE dysfunction leading to serous retinal detachment. While acute CSCR can be observed and is self-resolving in most cases, progression to chronic CSCR warrants treatment. The mainstay of treatment is currently photodynamic therapy, however treatment with SML or mineralocorticoid antagonists such as eplerenone are gaining momentum.