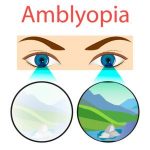
Amblyopia, often referred to as “lazy eye” is a significant neurodevelopmental visual disorder characterized by reduced vision that cannot be fully corrected solely by optical means or by removing ocular anomalies or pathologies.
Definition and Developmental Nature: Amblyopia is a developmental disorder of spatial vision that arises from abnormal visual input during critical periods of visual development, typically early in life. If the same visual input abnormalities occur later in life, amblyopia typically does not develop. The concept of amblyopia as a developmental disorder was first articulated by Worth in 1903. The term “amblyopia” translates from Greek as “dimness” or “dullness of vision” accurately describing the outcome, which is not blindness but rather a distortion and muddling of cortical connections. The severity of amblyopia appears to be directly related to how early the amblyogenic event occurs and how long it is present before treatment. Abnormal sensory experience during these early years can lead to “markedly disturbed cortical function” with evidence pointing to contrast sensitivity issues in cortical neurons for anisometropic amblyopia and significant loss of cortical connections for strabismic amblyopia.
Prevalence and Societal Impact: The prevalence of amblyopia is estimated to range from 1% to 5% of the general population, with a general estimate often cited around 3.5%. Despite these variations, amblyopia is considered the leading cause of monocular blindness in adults and the most frequent visual deficit in children. It is responsible for permanent vision loss in 2.9% of adults and contributes to a tenfold increase in the risk of monocular visual dysfunction compared to other childhood visual impairments. The condition carries a profound psychological and socioeconomic burden, impacting spatial perception, learning efficacy, and academic performance. It can limit career choices (especially those requiring high visual standards) and driving ability. Associated disabilities may include misjudging near and intermediate distances, reduced fine motor skills, clumsiness, and psychological impacts such as somatization, interpersonal sensitivity, obsession-compulsion, anxiety, and depression. There is a recognized need for increased understanding of the functional impact of amblyopia, as the lack of research in this area is considered “stunning”, which may lead to healthcare resources being diverted to conditions with firmer evidence of significant disability and effective treatment. There is also a reported increased risk of individuals with amblyopia losing vision in the fellow eye compared to those without amblyopia.
Classification and Etiology Amblyopia is primarily classified based on its underlying causes, known as amblyogenic factors. The main types include:
Strabismic Amblyopia: This is caused by a constant misalignment of the eyes (strabismus), which leads to binocular misregistration and active suppression of the image from one eye to avoid confusion or diplopia. This type often involves a greater foveal deficit, particularly in esotropic amblyopia. Strabismic amblyopia is highly associated with eccentric fixation, where the eye does not use the fovea for fixation, and the patient’s sense of “straight ahead” may shift to this extrafoveal point.
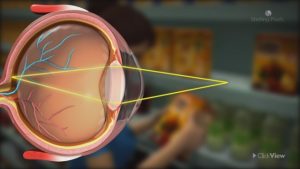
Anisometropic Amblyopia: This is the most prevalent form, accounting for approximately 50% of amblyopia cases. This results from a significant difference in refractive error between the two eyes, leading to unequal image degradation and consequently an unclear image from one eye. Hyperopic anisometropia is more commonly associated with amblyopia than myopic anisometropia. For instance, a patient with hyperopic anisometropia greater than 2.50 dioptres has a 50% chance of developing amblyopia, increasing to 100% with a difference greater than 4.50 dioptres. Suppression occurs to eliminate this blurred image. Prognosis for treatment is generally better for pure anisometropic amblyopia compared to mixed types. While some studies suggest it is the most common cause, others report it as the least prevalent pure type, with many cases being mixed.
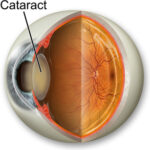
Form Deprivation Amblyopia: This type is caused by a physical obstruction of the visual axis, such as cataracts, ptosis (drooping eyelid), or corneal opacities. It has historically been referred to as “amblyopia of disuse”. The earlier the deprivation occurs and the longer it is
present, the greater the likelihood of amblyopia developing.
Isoametropic Amblyopia: A less common form resulting from high, symmetrical refractive errors in both eyes, particularly significant hyperopia or astigmatism. It is estimated to account for approximately 2% of nonstrabismic amblyopia.
Mixed Amblyopia: This involves a combination of strabismic and anisometropic factors and typically carries the worst prognosis for treatment outcomes. Other associated factors include astigmatism (sometimes leading to meridional amblyopia), nystagmus-related amblyopia, and high myopia. It is also crucial to note that functional amblyopia can be superimposed on vision loss caused by structural anomalies (e.g., optic nerve coloboma, optic nerve hypoplasia). In such cases, a trial of amblyopia therapy is often indicated. Affected Visual Functions While reduced visual acuity is the hallmark of amblyopia, it impacts a wide spectrum of visual functions beyond simple resolution:
Visual Acuity: Although reduced, acuity still generally peaks at the fovea in amblyopic eyes, but the overall resolution capacity is lower than normal. The extent of acuity loss can vary depending on the target used, with “crowding effects” (where single letters are seen better than
letters in a line) being a common phenomenon. Amblyopic eyes are often at their functional worst under photopic (bright light) conditions, displaying characteristics similar to a dark- adapted normal eye.
Contrast Sensitivity: Amblyopia typically leads to reduced contrast sensitivity for high spatial frequencies (fine detail), with less impact on low spatial frequencies (coarse forms). This loss can extend across the visual field and tends to increase with the severity of amblyopia, suggesting a neural rather than optical or oculomotor basis.
Hyperacuity and Spatial Perception: Hyperacuity tasks, such as Vernier acuity (ability to detect misalignments), are markedly degraded in amblyopia. Patients may experience monocular spatial distortion, spatial uncertainty, and difficulties with form and shape perception. These distortions are particularly common in strabismic amblyopia.
Fixation and Eye Movements: Amblyopic eyes often exhibit unsteady fixation, including increased drift amplitude and eccentric fixation (not using the fovea for fixation). Saccadic eye movements (rapid eye shifts) can also be defective, showing increased latency and reduced peak velocity. Overall, the amblyopic eye may track objects less accurately and be less effective for directing hand movements.
Accommodation: A reduced accommodative amplitude is a consistent finding in amblyopic eyes, potentially due to either afferent (sensory input) or efferent (motor output) defects.
Binocularity: Deficient or absent disparity vergence and subnormal binocularity are common. Interocular suppression, a key deficit in amblyopia, plays a significant role in disrupting binocular vision and is closely linked to deficits in visual acuity and stereopsis. Diagnosis Clinical diagnosis of amblyopia involves a comprehensive assessment to characterize the condition. This includes:
History Taking: Detailed questioning about strabismus, refractive history, and social history.
Visual Acuity Assessment: Measurement of visual acuity using various charts and tests, including single, crowded, and positional optotypes. Techniques may include Snellen charts, Bailey-Lovie chart, Tumbling E, Picture cards, and objective measures like Visually Evoked Potentials (VEP).
Fixation Evaluation: Assessment of fixation status and eye movements using methods like visuoscopy or the Haidinger Brush test to detect eccentric fixation.
Other Visual Functions: Evaluation of accommodation, monocular sensory perception, and binocular function. Contrast sensitivity testing is also crucial for treatment evaluation.