Introduction:
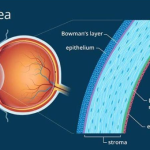
Keratoconus is a condition of the eye in which the normally rounded cornea bulges outward into a cone shape. The cornea is the clear, central part of the front surface of the eye. It protects your eye and helps you focus for clear vision. You pronounce keratoconus as care-ah-ta-KO-nus. Eye Care providers normally find keratoconus during your teenage years or your 20s and 30s, but it can also start in childhood. In some cases, a provider will diagnose a mild case of keratoconus at a later age. The changes in the shape of the cornea occur over several years but happen at a more rapid rate in younger people.
Symptoms:
The main symptoms of keratoconus include:
Gradually worsening vision in one or both eyes. (Generally, keratoconus affects both eyes.)
Having double vision when you look out of just one eye.
Seeing halos around bright lights.
Being sensitive to light. (The term for this sensitivity is photophobia.)
Having vision that gradually becomes distorted. With distorted vision, straight lines might look curvy or bent, and objects don’t have their correct shape.
Causes :
The cause of keratoconus is largely unknown. Some studies have found that keratoconus runs in families, and that it happens more often in people who have certain medical conditions.
In most cases, you don’t have an eye injury or a disease that leads to keratoconus. People with keratoconus tend to rub their eyes a lot, which may cause the condition to develop more rapidly.
Complication :
Potential complications of keratoconus include:
Corneal scarring: Scars develop on the cornea.
Corneal hydrops: Your cornea swells up with fluid suddenly.
Fleischer rings: Iron deposits cause rings within your cornea.
Vision loss: Vision loss can be mild or severe.
Diagnosis and Tests :
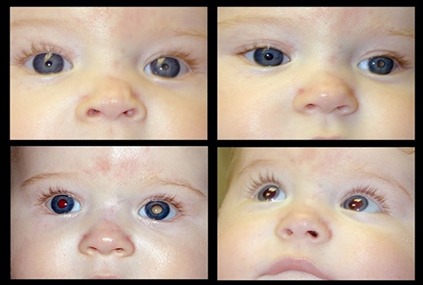
Visual acuity : This exam includes the Snellen eye chart and the one that has you looking through an instrument (phoropter) that helps you find your correct prescription for clear vision.
Slit lamp examination : This test combines a bright light and a microscope.
Keratometry: This test measures corneal shape and astigmatism.
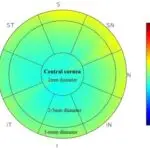
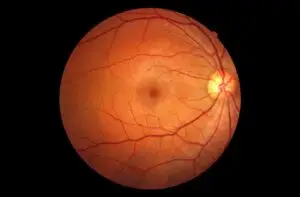
Corneal mapping (tomography and topography): These tests measure the curve of the surface of your eye and produce a “map” of your cornea. Keratoconus shows up on these tests.
Management and Treatment :
There are several methods for treating keratoconus, depending on how severe the condition is. Your eye care provider can help to decide which, if any, of these treatments may help you. Treatments include eyeglasses, contact lenses, implantable ring segments, corneal crosslinking and cornea transplant. Eyeglasses and contact lenses to treat keratoconus :
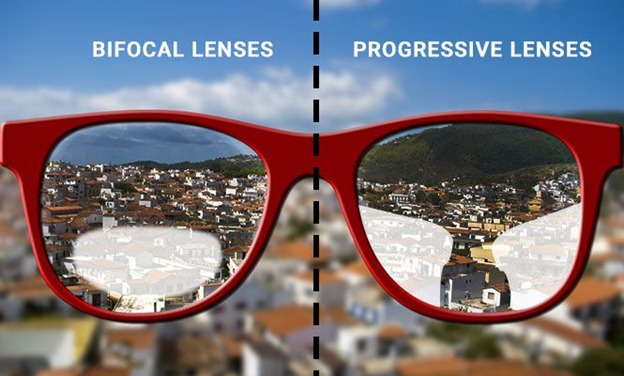
In the early stages of the disease, you can correct vision with normal eyeglasses or soft contact lenses. As keratoconus gets worse, eyeglasses may not correct your vision because of the amount of irregular astigmatism. You may need a special type of hard contact lens.
Corneal crosslinking to treat keratoconus :
Corneal crosslinking uses ultraviolet (UV) light treatment that may slow or stop the keratoconus from getting worse. In this procedure, you also receive local anesthesia. Your provider puts drops of a drug containing riboflavin (vitamin B2) into your eye for up to 30 minutes. Then, your provider exposes your eye to an UV light for up to 30 minutes. The purpose of corneal crosslinking procedure is to strengthen the bonds between your cornea’s collagen fibers and surrounding proteins. This can help keep
your cornea’s shape from getting steeper. Implantable ring segments (INTACS) to treat keratoconus: INTACS are small devices your provider inserts into your cornea to improve vision or make it easier to fit you with contact lenses. Your provider performs this procedure while you’re under local anesthesia (drops numb your eye). Then, your provider creates channels in the cornea and inserts the rings into these channels. The rings help to flatten the cornea and partially correct the cone shape the keratoconus causes.
Cornea transplant to treat keratoconus:
Your provider may suggest that you have a Cornea transplant if you have keratoconus that’s advanced. They’ll replace your diseased cornea with corneal tissue from a human donor. Usually, people with keratoconus have better vision after the transplant, but it may take more than a year for vision to stabilize. Some people may still need a specialty contact lens after the transplant to get their best vision.
Complications :
Eye pain or irritation.
Dry eyes
Keratoconus getting worse. Infection.
Potential complications from INTACS include: Infection.
Issues with glare or halos.
Corneal thinning. Potential complications related to cornea transplant include:
Cornea graft rejection.
Infection.
Glaucoma.
Potential complications or side effects from glasses or contact lenses are rare, but can happen. Let your provider know if you have any redness or discomfort in your eyes.