CONCOMITANT STRABISMUS
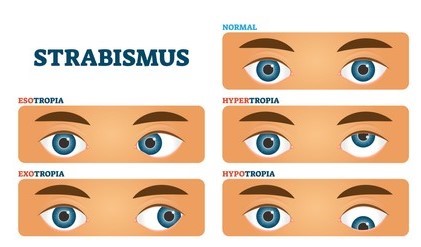
1) It is a type of manifest squint, wherein the angle of deviation in the squinting eye remains same in all directions of gaze.
2) Causes of development- the process of binocular vision and coordination of the ocular movements starts by the age of 3-6 months of birth and is completed by the age of 6-7 years. Therefore, any obstacle to the development of these process may result in concomitant strabismus. These obstacles are like- sensory, motor and central.
• Sensory obstacles includes refractive errors, prolonged use of incorrect spectacle, anisometropia, corneal opacities, lenticular opacities, obstruction in the pupillary area due to congenital ptosis.
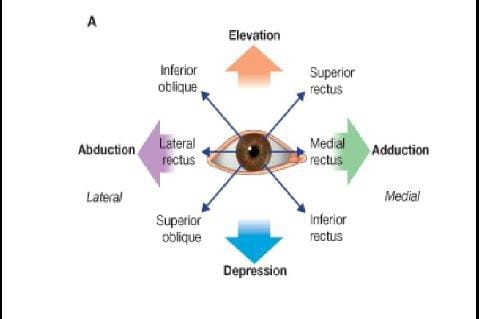
• Motor obstacles includes abnormalities of extraocular muscles, congenital abnormalities of the shape and size of the orbit, abnormalities of accommodation, convergence.
• Central obstacles includes abnormalities of cortical control of ocular movements, deficient development of fusion faculty.
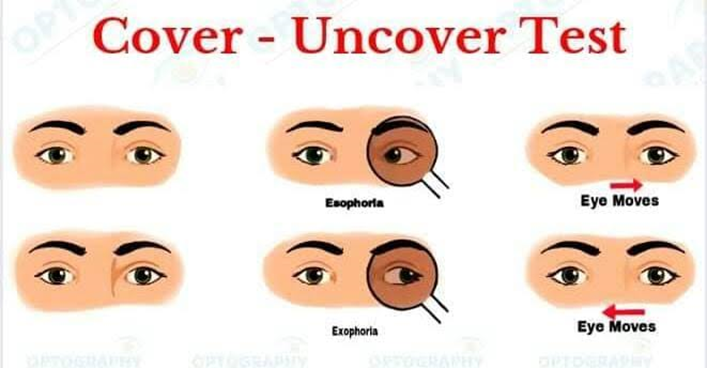
3) PRIMARY DEVIATION of the squinting eye is EQUAL to SECONDARY DEVIATION of normal eye under cover when patient fixes with squinting eye.
4) Ocular movements are normal and there is no limitation in any direction.
5) Angle of squint is usually constant in all direction of gaze.
6) Usually there is no diplopia. It is because of sensory adaption i.e. suppression, amblyopia or abnormal retinal correspondence. In adult life diplopia may occur spontaneously after surgical treatment.
7) Suppression and amblyopia may develop as sensory adaption to strabismus. Amblyopia develops in long standing monocular strabismus only and is responsible for poor visual acuity. Suppression may be in monocular squint and in alternating squint.
8) There is no abnormal head posture, as the angle of deviation is neutral and there is no diplopia.
9) There is no false projection of object, as the primary deviation is equal to the secondary deviation.
10) Investigation- Worth’s four-dot test to diagnose the presence of suppression and abnormal retinal correspondence in concomitant squint. In Worth’s four-dot test, if patient sees the two red lights, then there is suppression of left eye present. If patient sees three green lights, then there is suppression of right eye present. In abnormal retinal correspondence patient sees all four dots, even in presence of concomitant manifest squint.
11) Treatment –
• Spectacles with full correction of refractive error should be prescribed to improve the visual acuity.
• After correcting the refractive error, the normal eye is occluded and the patient is advised to use the squinting eye, occlusion therapy is indicated in the presence of amblyopia and it helps to improve vision in children below the age of 10 years.
• Preoperative orthoptic exercises are given to overcome suppression. And postoperative orthoptic exercise are required to maintain binocular single vision.
• Surgical treatment is required in most of the cases to correct the deviation. It should be done after correction of refractive error, treatment of amblyopia and after orthoptic exercises. Surgical result is usually good.
PARALYTIC STRABISMUS
1) It is a misalignment of the visual axes as a result complete or incomplete paralysis of one or more extraocular muscles.
2) Causes of development- the lesions may be neurogenic, myogenic and neuromuscular junction.
Common cause of neurogenic lesions are hypoplasia or absence of nucleus is a known cause of 3rd and 6th cranial nerve paralysis.
Cerebrovascular accidents (CVA) are more common in elderly people. Ophthalmoplegic migraine is a well-known vascular condition characterized by recurrent attacks of headache associated with paralysis of 3rd, 4th, 6th cranial nerve.
Traumatic lesions include head injury and direct or indirect trauma to the nerve trunks. Head injury is common cause of 4th and 6th nerve paralysis.
Toxic lesions include carbon monoxide poisoning, effects of diphtheria toxins, alcoholic and lead neuropathy.
3) SECONDARY DEVIATION of the normal eye is GREATER THAN PRIMARY DEVIATION of the squinting eye under cover, when the patient is made to fix with the squinting eye. This is due to the fact that the strong impulse of innervation required to enable the eye with paralyzed muscle to fix is also transmitted to the yoke muscle of the sound eye resulting in a greater amount of deviation. This is based on Hering’s law of equal innervation of yoke muscles.
4) Ocular movements are limited in the direction of action of paralyzed muscles.
5) Angle of squint is variable in different direction of gaze. Ocular deviation is typically sudden onset.
6) Diplopia present. It is the main symptom and most marked when the eye is rotated in the field of action of paralyzed muscle. Paralytic squint in an adult with previously single binocular vision, causes diplopia. It occurs due to formation of image on dissimilar points of two retina.
7) Amblyopia absent. Usually the paralytic squint develops in adults when visual acuity has already developed. As the visual acuity is normal in both eye, amblyopia is not developed. If it occurs in children below 6 years then amblyopia can occur.
8) A particular head posture is present depending upon the paralyzed muscle and head is turned towards the direction of action of the paralyzed muscle. It is adopted to neutralize the angle of deviation, or to separate the images maximally, so as to avoid diplopia.
9) False orientation of object is present due to increased innervational impulse conveyed to the paralyzed muscle. Object is projected too far in the direction of paralyzed muscle, due to increase in secondary deviation.
10) Investigation- Worth’s four-dot test to diagnose the presence of diplopia in paralytic squint. If patient sees two red lights and three green lights, then there is diplopia present.
Treatment- an exhaustive investigative work-up should be done to find out the cause of paralysis.
11) Treatment of diplopia that includes occlusion of affected eye temporarily and suitable prism correction for minor diplopia.
Observation for a period of 6 months for self-improvements.
Surgical treatment should be carried out in case the recovery does not occur in 6 months. But, surgical result is not satisfactory and at times, surgery should not use because of it may be harmful to the person.