Introduction
In the world of optometry, precise vision correction is both an art and a science. Among the
many techniques used by eye care professionals, retinoscopy stands out as a fundamental yet
powerful tool for determining refractive errors. Whether you're an aspiring optometrist, a
patient curious about eye exams, or a vision enthusiast, understanding retinoscopy can give you
valuable insights into how perfect vision correction is achieved.
What Is Retinoscopy?
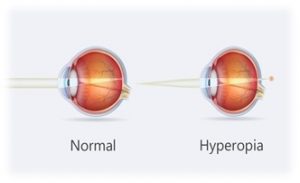
Retinoscopy is an objective method used by optometrists and ophthalmologists to measure a
patient’s refractive error—nearsightedness (myopia), farsightedness (hyperopia), astigmatism,
and presbyopia. Unlike subjective refraction (where patients respond to "Which is better, 1 or
2?"), retinoscopy relies on the examiner’s observation of light reflexes in the patient’s eyes.
How Does It Work?
The optometrist uses a retinoscope, a handheld instrument that projects a beam of light into
the patient’s eye. By observing how the light reflects off the retina, the examiner can determine
the eye’s focusing error. The patient looks at a distant target (to relax accommodation), while
the doctor moves the retinoscope beam across the pupil and observes the movement of the
reflected light.
– With Motion (Against Motion): Indicates hyperopia (farsightedness).
– Against Motion (With Motion): Indicates myopia (nearsightedness).
– Neutrality: The point where no movement is seen, indicating the correct lens power.
By placing different lenses in front of the eye until neutrality is achieved, the doctor accurately
determines the prescription needed for glasses or contact lenses.
Types of Retinoscopy
Retinoscopy techniques vary based on the light source and methodology used. The two main
types are:
1. Static Retinoscopy.
This is the most common form, performed when the patient’s eye is at rest (focusing on a
distant target). It measures the baseline refractive error without interference from the eye’s
focusing mechanism (accommodation).
2. Dynamic Retinoscopy.
Unlike static retinoscopy, dynamic retinoscopy assesses how the eyes focus at near distances. It
helps diagnose accommodative disorders, such as:
– Accommodative insufficiency (difficulty focusing up close)
– Presbyopia (age-related near vision loss)
Dynamic retinoscopy is particularly useful for prescribing reading glasses or bifocals.
The Retinoscope: A Closer Look at the Tool
The retinoscope comes in two main designs:
1. Streak Retinoscope
– Projects a linear "streak" of light
– Allows precise detection of astigmatism by aligning the streak with the eye’s principal
meridians
– Most commonly used in modern optometry
2. Spot Retinoscope
– Projects a circular spot of light
– Less commonly used today but still valuable in certain cases
Both types help determine refractive errors, but streak retinoscopes offer better accuracy for
astigmatism correction.
Step-by-Step Retinoscopy Procedure
Here’s how an optometrist performs retinoscopy:
Step 1: Preparation.
– The patient sits in a dimly lit room to enhance the visibility of the retinoscope’s light reflex.
– The doctor positions themselves about an arm’s length away (67 cm for optical infinity).
Step 2: Observing the Red Reflex.
– The retinoscope beam is shone into the patient’s eye, creating a red-orange reflex in the pupil
(similar to the "red-eye" effect in photos).
Step 3: Determining Refractive Error.
– The doctor sweeps the beam horizontally and vertically, observing the reflex movement.
– Based on the movement (with/against/neutral), trial lenses are introduced to neutralize the
reflex.
Step 4: Fine-Tuning for Astigmatism.
– If astigmatism is present, the streak is rotated to find the principal meridians, and cylindrical
lenses are used for correction.
Step 5: Final Prescription.
– Once neutrality is achieved, the lens power in the trial frame gives the patient’s approximate
prescription, which is later refined with subjective refraction.
Why Retinoscopy Is Still Essential in Modern Optometry
Despite advancements in autorefractors and digital eye testing, retinoscopy remains a gold standard because:
1. Works for Non-Verbal Patients.
– Ideal for infants, children, and individuals with communication difficulties.
2. Detects Subtle Refractive Errors.
– More accurate than autorefractors in high prescriptions and irregular corneas (e.g., keratoconus).
3. No Patient Input Required.
– Unlike subjective refraction, retinoscopy doesn’t rely on patient responses, reducing bias.
4. Cost-Effective and Portable.
– Unlike expensive machines, a retinoscope is affordable and usable in remote areas.
Common Challenges in Retinoscopy
While retinoscopy is highly effective, it requires skill and practice. Some challenges include:
– Uncooperative Patients: Children or individuals with involuntary eye movements can make the
test difficult.
– Media Opacities: Cataracts or corneal scars can obscure the red reflex.
– High Refractive Errors: Extreme myopia or hyperopia may require additional lenses for
accurate measurement.
Despite these hurdles, experienced optometrists can obtain reliable results with retinoscopy.
Conclusion
Retinoscopy is more than just a routine eye test—it’s a cornerstone of optometric practice. By
mastering this technique, eye care professionals ensure precise vision correction, especially in
cases where technology falls short.
Whether you’re an optometry student perfecting your streak technique or a patient wondering
how your eye doctor determines your prescription, retinoscopy remains the secret weapon behind perfect vision correction.
Next time you sit for an eye exam, appreciate the skill behind that flickering light—it’s the key
to seeing the world in sharp focus.