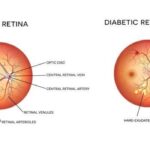
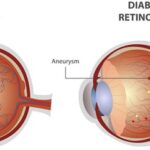
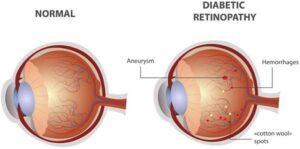
Early Diabetic Macular Edema (DME) is often difficult to identify clinically, especially in mild cases. It can be diagnosed using a combination of visual acuity tests, dilated eye exams, and imaging techniques like Optical Coherence Tomography (OCT) and Fundus Fluorescein Angiography (FFA).
The prevalence of diabetic macular edema is about 4-28%and about 2% of diabetic population is blind as a result of retinopathy.
• The best predictor of diabetic retinopathy is the duration of diabetes. There is no clinically apparent diabetic macular edema for 5 years after initial diagnosis.
• The severity of the diabetic maculopathy , generally parallels the duration of the disease and the adequacy of its control and not the severity of the diabetes.
• The incidence of diabetic retinopathy is more with insulin dependent diabetes mellitus (IDDM) than with non-insulin dependent diabetes mellitus (NIDDM), but the severity of maculopathy is more with NIDDM.
The course and severity of DR are affected by the presence of nephropathy, systemic hypertension, pregnancy, and positive family history of DR.
Here’s a more detailed breakdown:
Symptoms:
• Blurred vision: This is a common symptom, as the swelling in the macula interferes with sharp, central vision.
• Distorted vision (metamorphopsia): Objects may appear wavy or distorted, particularly when looking straight ahead.
• Reduced color vision: Patients may experience difficulty distinguishing colors.
• Reduced contrast or color sensitivity: This means objects may appear less vibrant or clear.
• Central scotoma: A blind spot in the center of vision, though this is more common with advanced DME.
• Worsening vision over time: DME can progress, leading to gradual vision loss.
Some patients may have excellent acuity with no visual complaints initially, especially if the central macula is only recently involved.
Diagnostic Test:
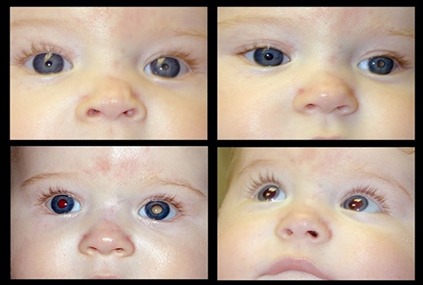
Visual Acuity Test: Determines how well a person can see at different distances using a standardized chart.
Dilated Eye Exam: Eye drops are used to widen the pupils, allowing the ophthalmologist to examine the retina more closely.
Optical Coherence Tomography (OCT): This imaging test provides detailed cross-sectional images of the retina, allowing for the measurement of retinal thickness and identification of edema (swelling).
Others test is FFA, Amsler Grid , slit lamp biomicroscopy etc.
Early Detection is Crucial:
Regular eye exams are essential for people with diabetes. Early detection and treatment can help prevent vision loss.
Even in the absence of symptoms, DME can be present. Regular eye exams are necessary to identify the condition before significant vision impairment occurs.
Early intervention can improve outcomes. Treatment options for DME include anti-VEGF therapy, steroids, and in some cases, surgery.
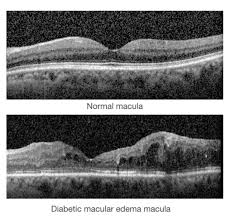
Diabetic macular edema detection with OCT
Early Diabetic Macular Edema (DME) can be identified with Optical Coherence Tomography (OCT) by observing changes in retinal thickness and the presence of intraretinal fluid. OCT provides detailed cross-sectional images of the retina, allowing for the detection of subtle changes in the macula, which may indicate the development of DME.
Here’s a more detailed look at how OCT aids in identifying early DME:
1. Retinal Thickening:
• Macular Thickness: OCT can measure the thickness of the retina, including the macula. In DME, the macula, the central part of the retina responsible for sharp central vision, can thicken due to fluid buildup.
• Foveal Depression: The fovea, the center of the macula, is normally a shallow depression. In DME, this depression may flatten or even disappear, indicating significant retinal thickening.
2. Intraretinal Fluid:
• Cystoid Spaces: OCT can visualize intraretinal cystoid spaces, which are fluid-filled spaces within the retina. These spaces are a hallmark of DME, particularly in the early stages.
• Hyporeflective Areas: Intraretinal fluid appears as hyporeflective areas (darker areas) on OCT scans, indicating the presence of fluid within the retinal layers.
3. OCT Biomarkers for Prognosis:
• Disorganization of Inner Retinal Layers: OCT can assess the integrity of the inner retinal layers. Disorganization, where the boundaries between different retinal layers are unclear, is an indicator of more severe edema and a poorer visual prognosis.
• Hyperreflective Foci: Hyperreflective foci in the retina, particularly in the inner retinal layers, can indicate leakage of subclinical lipoproteins or other materials, potentially affecting visual prognosis.
4. OCT Angiography (OCT-A):
• Microvascular Alterations: OCT-A, a specialized form of OCT, can visualize the retinal vasculature. In DME, OCT-A can reveal alterations in the macular and peripapillary capillary networks, helping to assess microvascular changes, retinal ischemia, and neovascularization.
In summary, OCT is a valuable tool for identifying early DME by detecting retinal thickening, intraretinal fluid, and other biomarkers. OCT-A can further enhance the evaluation by visualizing microvascular changes in the retina.