The human eye is a complex and delicate organ, and every part of it plays an important role in maintaining clear vision. One such important aspect of eye health is central corneal thickness. The
thickness of the cornea, especially at its center, is crucial for diagnosing and managing various eye
diseases, including glaucoma, keratoconus, and refractive errors. Understanding central corneal
thickness and its significance can help in detecting eye conditions early and ensuring proper treatment.
What is Central Corneal Thickness
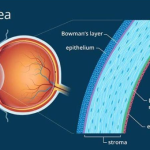
The cornea is the transparent outer layer of the eye that helps focus light onto the retina. The central part of the cornea is called central corneal thickness. In most healthy adults, this thickness ranges between 500 and 600 microns. However, the thickness can vary from person to person due to factors such as age, genetics, ethnicity, and overall eye health.
To measure central corneal thickness, eye doctors use different techniques. Some of the most common
methods include:
1. Pachymetry- which is widely used and includes two types:
Ultrasound pachymetry, where a small probe is placed gently on the cornea to measure its thickness
Optical pachymetry, which uses light waves to measure thickness without direct contact
2. Scheimpflug imaging- which is a non-contact method that creates a three-dimensional image of the cornea
3. Optical coherence tomography- which is a laser- based imaging technique that provides detailed cross-sectional images of the cornea
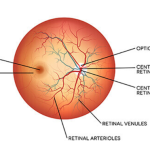
The Importance of Central Corneal Thickness in Glaucoma
Glaucoma is an eye disease that damages the optic nerve and can lead to permanent vision loss. The
damage is usually caused by high pressure inside the eye. Central corneal thickness plays a key role in
the diagnosis and treatment of glaucoma in the following ways:
Influence on eye pressure readings
Eye pressure is measured using a test called Goldmann applanation tonometry. This test assumes
an average corneal thickness of 540 microns. If the cornea is thicker than normal, the test may show a
higher-than-actual eye pressure reading. If the cornea is thinner than normal, the reading may be
lower than the actual eye pressure. This means a person with a thin cornea could have undiagnosed glaucoma because their real eye pressure is higher than what the test shows.
Risk factor for glaucoma progression
Studies have shown that people with thin corneas are at a higher risk of developing glaucoma. This is
because a thinner cornea may indicate weaker eye structures, making the optic nerve more vulnerable to pressure-related damage.
Measuring central corneal thickness helps eye doctors get a more accurate understanding of a
patient’s eye pressure. It also helps in identifying people who are at a higher risk of glaucoma,
allowing for earlier treatment and better disease management.
Central Corneal Thickness and Keratoconus
Keratoconus is a progressive disease in which the cornea becomes thin and cone-shaped, leading to
blurred and distorted vision. Central corneal thickness is a key factor in diagnosing and monitoring this condition.
Early diagnosis
In a normal eye, the cornea has a thickness of more than 500 microns. In people with keratoconus, the
cornea becomes thinner, sometimes dropping below 400 microns. Measuring central corneal thickness
helps detect keratoconus early, even before vision problems become severe.
Impact on treatment options
A procedure called corneal cross-linking is often used to strengthen the cornea in keratoconus
patients. However, if the cornea is too thin, this procedure may not be safe. Knowing the corneal thickness helps doctors decide whether a patient is a suitable candidate for treatment.
Differentiating from other conditions
Other corneal conditions, such as pellucid marginal degeneration, can also cause corneal thinning.
Measuring central corneal thickness along with other tests helps doctors distinguish between different
conditions and choose the best treatment plan.
Central Corneal Thickness in Refractive Surgery
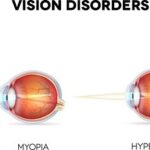
Refractive surgeries like LASIK and PRK are used to correct vision problems such as nearsightedness,
farsightedness, and astigmatism. These procedures involve reshaping the cornea using a laser. Central
corneal thickness is an important factor in determining whether a person is eligible for these
surgeries.
Minimum corneal thickness requirement
In LASIK, a thin flap is created on the cornea, and the laser reshapes the tissue underneath. If the
cornea is too thin, performing LASIK can weaken it and lead to complications like corneal ectasia, a
condition where the cornea bulges forward and causes vision problems. If a person’s cornea is too
thin for LASIK, doctors may recommend an alternative procedure such as PRK, which does not
require creating a flap.
Customized treatment planning
For patients with thinner corneas, doctors may need to adjust the laser treatment to preserve corneal
stability. Measuring central corneal thickness helps in planning the safest and most effective surgical
approach.
Before undergoing LASIK or PRK, every patient should have a corneal thickness test to ensure they
are suitable candidates for the procedure.
Central Corneal Thickness in Corneal Edema and Eye Injuries
Corneal edema
When the cornea swells due to fluid buildup, it becomes thicker than normal. This condition is
known as corneal edema and can occur due to factors like aging, eye surgery, or inflammation.
Measuring central corneal thickness helps doctors track the severity of corneal edema and determine if
treatment is needed.
Eye injuries
In cases of eye trauma, the cornea may temporarily swell. Monitoring corneal thickness after an injury
helps in detecting complications such as scarring or infections.
Variations in Central Corneal Thickness Across Different Populations
Research has shown that central corneal thickness can vary among different ethnic groups.
People of African and Asian descent tend to have thinner corneas, which may put them at a higher risk
of glaucoma
People of Caucasian and Hispanic descent generally have thicker corneas, which can affect eye
pressure readings
Understanding these variations helps eye doctors assess glaucoma risk more accurately and provide better care for different populations.
Why Regular Monitoring of Central Corneal Thickness is Important
Central corneal thickness is not just a measurement; it is an important indicator of eye health. It plays a role in diagnosing glaucoma, detecting keratoconus, determining eligibility for refractive surgery, and monitoring corneal conditions.
Key reasons why measuring central corneal thickness is important
1.Helps in accurate diagnosis of glaucoma
2.Detects and monitors keratoconus progression
3.Ensures safe and effective refractive surgery
4.Identifies corneal swelling and other abnormalities
Since corneal thickness remains stable in most people throughout life, a single measurement can
provide valuable insight into a person’s eye health. For those at risk of eye diseases or considering laser eye surgery, checking central corneal thickness is a simple but important step in protecting vision.
Regular eye checkups, including corneal thickness measurement, can help detect problems early and
ensure timely treatment, preserving clear and healthy vision for years to come.