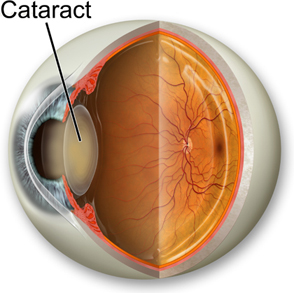
A juvenile cataract, also known as a pediatric cataract, refers to a lens opacity that occurs in children and young adults. Unlike age-related cataracts, which typically develop later in life, juvenile cataracts can appear at any time from birth to early adulthood. They can significantly impact vision and quality of life, making early diagnosis and appropriate treatment crucial.
Understanding Cataracts
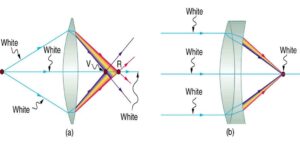
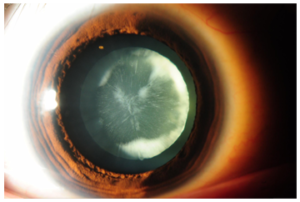
To understand juvenile cataracts, it’s essential to first grasp what a cataract is. The lens of the eye is a transparent structure that helps focus light onto the retina at the back of the eye. A cataract occurs when this lens becomes cloudy or opaque, impairing vision. In juvenile cataracts, this clouding happens during childhood or adolescence, often due to various factors that may be congenital or acquired.
Types of Juvenile Cataracts
Juvenile cataracts are categorized based on their cause and the age of onset:
Congenital Cataracts: These are present at birth or develop shortly after. They may be inherited or result from prenatal factors, such as infections or genetic abnormalities.
Acquired Cataracts: These develop due to external factors such as trauma, systemic diseases, or medication use. In some cases, they are associated with other ocular or systemic conditions.
Developmental Cataracts: These occur when the lens develops abnormally during childhood. Unlike congenital cataracts, they might not be present at birth but become evident as the child grows.
Causes and Risk Factors
The causes of juvenile cataracts can be broadly categorized into genetic and environmental factors:
Genetic Factors: Many juvenile cataracts are inherited in an autosomal dominant or recessive manner. Mutations in specific genes that regulate lens development can lead to cataract formation. Syndromic cataracts, associated with genetic conditions like Down syndrome or Lowe syndrome, are also observed.
Environmental Factors: Prenatal factors such as maternal infections (e.g., rubella, toxoplasmosis) or exposure to certain drugs or toxins can result in congenital cataracts. Postnatal factors include trauma, prolonged use of certain medications like corticosteroids, or diseases like diabetes.
Symptoms
The symptoms of juvenile cataracts can vary depending on the severity and type of cataract. Common symptoms include:
Visual Impairment: The most significant symptom is reduced vision. Children might exhibit signs of poor visual acuity, difficulty with reading, or clumsiness.
Glare and Light Sensitivity: Children may complain of glare or light sensitivity, especially in bright environments.
Strabismus: Misalignment of the eyes, or strabismus, can occur as the child’s vision becomes impaired.
Nystagmus: Some children may develop involuntary eye movements known as nystagmus.
In infants and very young children, symptoms might be less obvious. Parents might notice that the child is not reaching visual milestones or has unusual eye movements.
Diagnosis
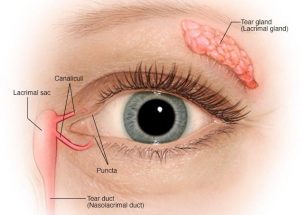
Early diagnosis of juvenile cataract is vital for effective management. Diagnosis involves a comprehensive eye examination performed by an ophthalmologist. Key steps include:
Medical History: A detailed history to identify any hereditary conditions, prenatal exposures, or other risk factors.
Eye Examination: Includes assessing visual acuity, eye alignment, and examination of the lens using techniques like slit-lamp microscopy.
Imaging: In some cases, imaging techniques like ultrasound may be used to evaluate the extent of the cataract and its impact on eye structures.
Treatment:
The management of juvenile cataracts depends on the cataract’s severity and the impact on vision:
Observation: In cases where the cataract is small and does not significantly impair vision or eye development, regular monitoring may be sufficient.
Surgical Intervention: For significant visual impairment, cataract surgery is often recommended. The surgical procedure involves removing the cloudy lens and usually replacing it with an artificial intraocular lens (IOL). In infants and very young children, this surgery is carefully planned to ensure optimal outcomes and proper lens power for visual development.
Postoperative Care: After surgery, follow-up care is critical to ensure proper healing and visual rehabilitation. This may include the use of corrective lenses or patching therapy to improve visual outcomes.
Management of Associated Conditions: If the cataract is part of a broader syndrome or associated with other health conditions, a multidisciplinary approach involving other specialists may be necessary.
Long-Term Outcomes
The prognosis for children with juvenile cataracts depends on several factors, including the timing of intervention, the type of cataract, and any associated conditions. Early diagnosis and treatment generally lead to better visual outcomes. Children who undergo successful cataract surgery and receive appropriate visual rehabilitation can often achieve near-normal vision.
Challenges and Considerations
Rehabilitation: Post-surgical visual rehabilitation can be challenging, particularly in very young children. Ensuring proper use of corrective lenses and addressing any visual development issues requires ongoing effort.
Complications: Potential complications of cataract surgery include infection, lens dislocation, or secondary cataract formation. Regular follow-ups are necessary to monitor and address any issues that arise.
Psychosocial Impact: The visual impairment associated with juvenile cataracts can affect a child’s development, academic performance, and social interactions. Support from educators and psychologists may be beneficial in helping children adjust.
Conclusion:
Juvenile cataracts are a significant ocular condition that can impact vision from an early age. Understanding their causes, symptoms, and treatment options is crucial for timely intervention and optimal visual outcomes. With advancements in surgical techniques and a multidisciplinary approach to care, children with juvenile cataracts can often lead successful and fulfilling lives. Early detection and comprehensive management are key to minimizing the impact of this condition and supporting the child’s overall development.
|
ReplyReply to allForward |