Keratoconus is a relatively rare eye condition that affects the structure of the cornea, leading to visual impairment. While it’s not a well-known condition, understanding its symptoms, causes, and treatment options is essential for those diagnosed with it and their loved ones.
What is Keratoconus?
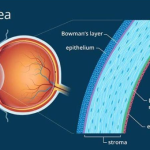
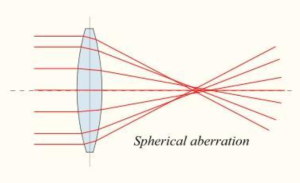
Keratoconus is a progressive disorder where the cornea, the clear, dome-shaped front surface of the eye,
gradually thins and bulges into a cone shape. This abnormal shape impairs the ability of the eye to focus
light properly onto the retina, resulting in distorted vision.
Symptoms:
A. -Blurred vision: One of the most common symptoms of keratoconus is blurred vision, which may worsen over time.
B.- Increased sensitivity to light (photophobia): Individuals with keratoconus may experience heightened sensitivity to light, making it uncomfortable to be in brightly lit environments.
C.- Frequent changes in prescription glasses or contact lenses: Due to the progressive nature of keratoconus, individuals may find that their prescription changes frequently as the condition worsens.
D.- Distorted vision: Straight lines may appear bent or wavy to individuals with keratoconus, making it difficult to perform tasks such as reading or driving.
E.- Difficulty seeing at night (night blindness): Many people with keratoconus also experience difficulty seeing clearly in low-light conditions, such as at night.
Causes:
The exact cause of keratoconus is not fully understood, but several factors may contribute to its development:
A.- Genetics: Keratoconus often runs in families, suggesting a genetic component to the condition.
B.- Eye rubbing: Rubbing the eyes vigorously may increase the risk of developing keratoconus.
C- Corneal thinning: A thinner cornea may be more susceptible to developing keratoconus.
D- Eye conditions: Certain eye conditions, such as retinitis pigmentosa, Down syndrome, and Ehlers-Danlos syndrome, are associated with an increased risk of keratoconus.
Diagnosis:
Diagnosing keratoconus typically involves a comprehensive eye examination, including:
A- Visual acuity test: This test measures how well you see at various distances.
B- Corneal topography: This imaging test creates a detailed map of the curvature of the cornea, helping to detect any abnormalities.
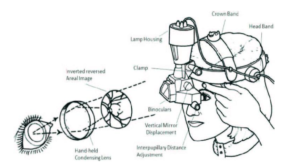
C- Slit-lamp examination: A slit lamp is used to examine the cornea closely for signs of keratoconus, such as thinning and scarring.
Treatment Options:
While there is currently no cure for keratoconus, several treatment options are available to help manage the condition and improve vision:
A- Glasses or contact lenses: In the early stages of keratoconus, glasses or soft contact lenses may be
sufficient to correct vision. As the condition progresses, rigid gas permeable (RGP) contact lenses may be
recommended to provide better vision by masking the irregular shape of the cornea.
B- Corneal collagen cross-linking (CXL): This minimally invasive procedure involves applying riboflavin (vitamin B2) eye drops to the cornea, followed by exposure to ultraviolet (UV) light. CXL strengthens the cornea and can help slow or stop the progression of keratoconus.
C- Intacs: Intacs are small, plastic rings that are surgically inserted into the cornea to flatten the cone-shaped bulge and improve vision.
D- Corneal transplant: In severe cases of keratoconus where other treatments are ineffective, a corneal transplant may be necessary. During this procedure, a surgeon replaces the diseased cornea with a healthy donor cornea.
Conclusion:
Keratoconus is a complex eye condition that can have a significant impact on a person’s quality of life if left untreated. However, with early diagnosis and appropriate treatment, many individuals with
keratoconus are able to manage their symptoms effectively and maintain good vision. If you’re
experiencing any symptoms of keratoconus or have concerns about your eye health, it’s essential to consult an eye care professional for a thorough evaluation and personalized treatment plan.